23 Sept 2019
Gian Marco Arcabasso and Francesc Xavier Salord Torres look at diagnostics and resolution methods regarding these types of jaw injuries in canine and feline patients.

Mandibular and maxillary fractures have an occurrence of 3% in dogs and 15% in cats, and commonly result from trauma. Approaching these patients in the context of polytrauma is highly advisable.
Different methods can be used for the resolution of mandibular and maxillary fractures, and have been classified into three groups – medical methods, interdental stabilisation techniques and surgical repair. The use of one or the other will depend on the lesion site, ability and skills of the surgeon, and financial capability of the owner.
For what concerns the diagnostic approach, conventional radiographs can be a good choice, but are sometimes not precise enough to show the fracture site properly. In these cases, dental radiographs and CT can be considered.
With an occurrence of 3% in canine patients and 15% in feline patients, jaw fractures are usually caused by a wide variety of traumas arising from road traffic collisions, fights between animals and high-rise syndrome in cats, among others (Umphlet and Johnson, 1988; 1990).
Therefore, approaching the patient as a polytraumatic individual must always be considered (Johnson et al, 2005). Other causes of mandibular and maxillary fractures are severe periodontitis, metabolic diseases and neoplasia (Fossum, 2012). Therefore, mandibular and maxillary fractures are unlikely to be clinically presented by themselves.
Similar techniques used for the treatment of long bone fractures can also be performed to repair mandibular and maxillary fractures. However, especial particularities should always be contemplated.
Placing fixing material without harming local blood vessels, nerves and dental roots are one of the challenges of repairing mandibular and maxillary fractures with conventional techniques (Snyder et al, 2016).

When an animal is presented with a mandibular and/or maxillary fracture, it is tempting to treat the fracture and disregard the patient as a whole. Jaw fractures may commonly occur associated with injury to other vital organs (Radke, 2016) and, therefore, have to be considered in the context of polytrauma (Johnson et al, 2005).
A thorough general, orthopaedic and neurological evaluation is extremely advisable prior to definitive approach of any musculoskeletal injury. The initial approach should be focused on major body system examination, with particular attention to respiratory and cardiovascular systems. Stabilisation should begin with the classic ABC:
In most cases, diagnosis of mandibular and maxillary fractures is simple, and only based on the results of the clinical exam and radiographs. In more difficult cases, overlapping of bony structures and skull complexity can make radiographs non-diagnostic.
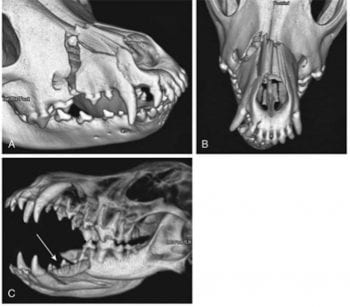
Radiographic examination could also be a challenge when it runs to find small fractures (Figure 1; Bar-Am et al, 2008). In these cases, CT scan is advisable (Figure 2). Usage of intramural dental radiographs would also reduce the risk of missing minor fractures and provide a better view of the roots of the teeth (Hale, 2015).
To relieve the pain is essential when dealing with trauma patients. Besides the importance for animal welfare, effective pain management is also likely to improve clinical outcomes (MacFarlane, 2018).
General rules applied to manage surgical pain are also suggested for dogs and cats undergoing mandibular and/or maxillary fracture repair surgeries.
These suggest the use of preoperative opioids plus a tranquiliser/sedative (for example, acepromazine and midazolam or diazepam and dexmedetomidine), followed by the administration of an NSAID either pre-operatively or postoperatively, based on patient risk factors and clinical preference (Epstein et al, 2015).
Loco-regional anaesthetics are also largely used. This combination can reduce the dose of other anaesthetic agents, decreasing the risk of adverse effects, such as intraoperatory hypotension.
One of the easiest nerve blocks to perform is the infraorbital nerve block, also indicated for tooth extractions and surgery of the nostrils. However, when it comes to dealing with mandibular and maxillary fractures, blocking maxillary and mandibular nerves is also recommended.
The maxillary nerve block is recommended for upper arcade tooth removal, maxillectomy and palate surgery, while the mandibular nerve block is indicated for mandibular tooth removal, mandibulectomy and mandibular mass excision. Blocks can be performed both intra-orally and extra-orally (Duke-Novakovski et al, 2016).
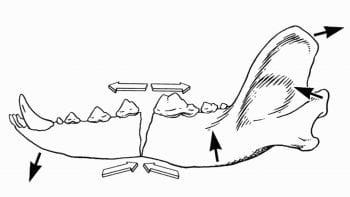
Generally, the idea of the techniques used to repair mandibular and maxillary bony lesions is based on the alveolar side tension-bend forces, both in the upper and lower jaws (Figure 3).
Because of this, performing a reduction of the fractures as close as possible to this margin is recommended. However, it is important to keep in mind that a just post-surgery functional occlusion is much more important than a good surgical reduction of the fracture (Harasen, 2008; DeCamp et al, 2016).
Placement of a tracheostomy tube might be necessary when fracture reduction is needed. As an alternative, a shorter endotracheal tube, which ends just behind the incisors, can also be helpful to avoid tracheostomies.
This final technique offers the possibility to disconnect the tube from the gas system during the surgery and check if dental occlusion is correct (Duke-Novakovski et al, 2016).
Different repair techniques are reviewed and summarised in this article.
An inexpensive fixation, adhesive fixation tape can be applied as a temporary fixation before surgery (preventing fracture displacement), after surgery (reducing range of motion) and to reduce fractures minimally displaced, where the healing is going to be rapid, and for those where a complex surgical approach may be difficult (Figure 4; Goeggerle et al, 1996). Other conditions in which tape muzzle is useful include pathologic fractures (for example, due to periodontal disease) or when other methods of fixation are not possible.
This technique consists of tethering the upper and lower jaws together with adhesive tape. This is mainly suitable for those fractures situated in the medium-caudal region, instead of the rostral part.
In some cases – especially in unstable fractures – muzzling tightly is necessary and normal feeding becomes impossible. Syringe feeding or placing a feeding tube (Goeggerle et al, 1996; DeCamp et al, 2016) are some of the recommended options in these cases.
Contact dermatitis caused by the tape is the main complication of this technique. It spontaneously resolves after the tape removal, though (Bennet et al, 1994).
Interdental fixation with acrylic-based systems is limited to use in mandibular and maxillary fractures occurring between intact canine and carnassial teeth. Acrylic-based polymer systems are extracortical devices designed to stabilise fractures and, unlike metal wires, these systems do not damage neovascular structures and dental roots (Legendre, 2003).
Teeth involvement into the system is one of the limitations of acrylic fixations. Enamel does not adhere well to acrylic. Therefore, prior to the application of these devices, enamel of the teeth in question – generally the canines – is usually treated with phosphoric acid to promote its adhesion to the material (Smith, 2004).
Acrylic intra-oral splints can be used without metallic reinforcement (Fossum, 2012). However, when combined, interdental wires with acrylic intra-oral splints provide the strongest fixation when tested in bending (Smith, 2004).
Bonding the maxillary and mandibular canine teeth together in anatomic alignment is an alternative to the tape muzzle for conservative fracture treatment. As aforementioned, the canine teeth need to be prepared, cleaned, pumiced and acid-etched before alignment with acrylic-based devices. The technique allows the mouth to open approximately 1cm (Fossum, 2012).
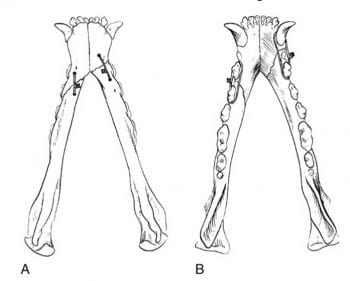
Interdental wires are placed around the teeth adjacent to the fracture line (Figure 5). To prevent the wire from slipping, interdental metallic devices may be placed through holes drilled in the maxillary or mandibular bone (Fossum, 2012). However, the wire can be also placed without drilling hard tissues adjacent to the fractures (DeCamp et al, 2016).
This technique is mainly used for the treatment of mandibular symphysis and body fractures (Harasen, 2008). Unfortunately, food accumulation and gingivitis induced by the wire material are common complications of this technique (Bennet et al, 1994).
Keeping the upper and lower jaws together is the main target of cerclage placement between the maxilla and mandible. This technique generally helps preserve the teeth roots. However, because sometimes the wiring can be kept tight, a feeding tube might need to be placed if the patient cannot have conventional enteral nutrition (DeCamp et al, 2016).
In case of non-comminute fractures with multiple and oblique fragments, interfragmentary wires are indicated. This technique is only considered ideal in cases of simple and reconstructible fractures (Fossum, 2013). Therefore, use of cerclage alone is almost never an excellent choice, whatever the pattern used is. This is because, during its placement, micro flexions of the thread are formed, which stretch in a few days after the surgery, leading to a loss of tension in the cerclage (Hale, 2015).
Mainly for comminuted and bilateral fractures, plates (generally made of titanium) offer an important immobilisation of the fracture segments. Thin and malleable devices are used, providing and preserving the necessary strength and permitting faster returns to normal function. However, application of plates can also be related to complications. Difficult preservation of dental roots, vascularisation and innervation is the main handicap of this technique (Hale, 2015).
External skeletal fixations are based on the application of a variable number of pins in each fracture fragment – generally two in the caudal aspect and one in the rostral fragment of the fracture. This technique particularly suits to non-union, multiple and bilateral fractures, as well as when lack of bony material exists (trauma caused by a gunshot, for example; Harasen, 2008).
To enable a functional reduction, the mouth has to be maintained closed. The first pin inserted is the most caudal one, followed by the application of the cranial one, which, in some cases, can deepen up to the other side of the mandible. Once the first two pins are placed, they are connected to the bar using clamps. Then more pins can be positioned (DeCamp et al, 2016). Interdental wiring can be used to add strength to the structure – especially in bilateral mandibular fractures.
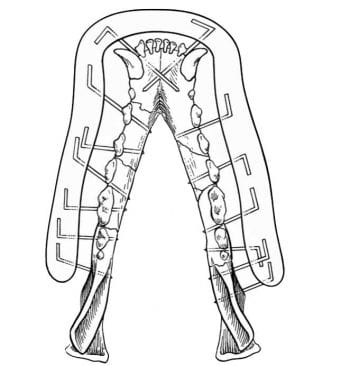
The external skeletal acrylic fixator method relies on the same principle as the metal fixator, with the only difference being the metal bar connecting pins and clamps is substituted by an acrylic device (Figure 6). This method allows the use of pins with reduced diameter, especially indicated to reduce comminute fractures composed by small fragments. Pins with a roughened surface have better performance to adhere to the acrylic composite. However, in its absence, a normal smooth pin can be used as long as its end is bent (DeCamp et al, 2016).
Proper management of the fracture is essential for the fixation of mandibular and maxillary fractures (Fossum, 2012). Due to the thickness of the maxillary bone in relation with the volume it occupies, and consequently the relative wider vascularisation, healing of maxillary fractures appears to be faster than mandibular bony injuries.
Mandibulectomy might be the only treatment warranted in cases of surgical failure and/or concurrent conditions, such as severe periodontal disease, mandibular non-union or malunion, severe comminution, osteomyelitis and presence of pathologic fractures (Goeggerle et al, 1996; Carvalho et al, 2015).
Malocclusion and its possible sequelae (periodontal disease, pain, dysphagia and temporomandibular arthritis) alongside osteomyelitis are two of the most common complications after a mandibular and/or maxillary fracture repair (Fossum, 2012). Antibiotics are normally used since most of the fractures observed are open.
Avoiding risky behaviours after the surgery (for example, playing with hard objects, bone chewing and so on) has to be strictly recommended to the owners to prevent post-surgery breakdowns (DeCamp et al, 2016).
Jaw fractures are usually caused by a wide variety of traumas. Therefore, evaluating the patient before concentrating on treating the fracture is essential to correctly manage a trauma patient. Unlike the fixation of long bone fractures, mandibular and maxillary fractures represent a bigger issue because of the anatomy and presence of loco-regional sensitive structures.
Postoperative functional occlusion is more important than a good reduction of the maxillary and/or mandibular fracture site. The prognosis for healing of mandibular and maxillary fractures is generally favourable if proper management of the condition has been carried out. However, malocclusion and osteomyelitis are two of the most common complications of mandibular and maxillary fracture repair.
This article tries to summarise most of the common techniques – used both in general practice and referral centres – to repair mandibular and maxillary fractures. We have deliberately decided to not report information about the success rate of each technique due to the lack of information and overlapping data population in this field. In addition, we consider the success rate will really depend on the skills and confidence of the surgeon.
Practical details – including the cost of techniques and materials used, as well as the duration of each procedure – are being excluded from this article due to extension limitations and evident international variations.