11 Jun 2018
Karen Perry takes a look at methods to treat this condition, including a variety of drugs.

Image: Lilli / Adobe Stock
Chronic pain has been defined in human medicine as lasting for more than three to six months (Merskey and Bogduk, 1986), but whether this timeline remains relevant to veterinary species when we consider their substantially shorter lifespan is questionable (Adrian et al, 2017).
Due to the difficulty in demarcating the transition from acute to chronic pain and the growing realisation these exist on a continuum rather than as discrete entities, alternative definitions have begun to be used that may be more useful in the context of understanding pain and how to treat it (Woolf, 2010) – adaptive and maladaptive.
Adaptive pain encompasses both nociceptive and inflammatory pain (Woolf, 2010). Nociceptive pain is only activated by high threshold noxious stimuli, including those that cause, or have potential to cause, tissue injury. Inflammatory pain occurs after tissue damage and results in increased sensitivity of the tissues associated with a classical inflammatory response.
Both of these types of pain are considered protective, or adaptive, pain in that they serve to sense and/or avoid actual or potential tissue damage (Adrian et al, 2017). These typically have an easily identifiable cause (such as surgery and injury), and are reversible. In contrast, maladaptive pain is not protective, and develops secondary to plastic changes in the pain processing system. It can be further subdivided into neuropathic pain, which results from direct damage to neural tissue, and functional pain, where in the absence of any neural lesions or inflammation, pain is driven by dysfunction or malfunction of the nociceptive system (Adrian et al, 2017).
Classically, neuropathic pain is defined as resulting from gross, obvious damage to the spinal cord or peripheral nerves, such as with peripheral nerve sheath tumours or surgical trauma. However, it is increasingly recognised many diseases, such as OA, may involve a degree of peripheral neuropathy via either direct damage to nerve endings present in the tissues or via increased innervation that accompanies joint remodeling and angiogenesis (Ivanavicius et al, 2007; Im et al, 2010; Bennett et al, 2012; French et al, 2017).
The obvious examples of functional pain are phantom limb pain or fibromyalgia – situations where increased sensitivity to stimuli and spontaneous pain are noted in the absence of any evidence of a lesion or inflammation. However, increasingly, it is recognised many conditions, such as OA, incorporate a component of functional pain – changes in the CNS function that heighten sensitivity or result in spontaneous pain.
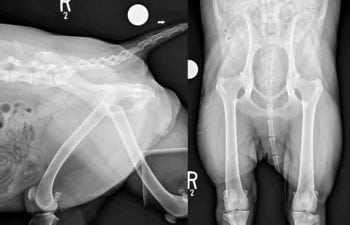
A maladaptive component to pain is believed to be present in up to 40% of human patients suffering from OA-associated pain (Crawford et al, 1998; Ivanavicius et al, 2007). It is important we recognise these different types of pain and appreciate one patient may be suffering from multiple different types, as this may well impact on the therapeutic regimen chosen (Adrian et al, 2017; Figure 1).
Although it may not be easy to recognise, any condition that results in chronic pain is likely to represent a complex mixture of adaptive and maladaptive pain. In OA, pain will consist of several different components, including an active sustained inflammatory component and maladaptive pain associated with neuronal changes and sensitisation (Lee et al, 2011; Woolf, 2010; Baron et al, 2013). In fact, it was shown dogs with OA have measurable central sensitisation indicative of maladaptive pain (Knazovicky et al, 2016). The driving condition starts and remains as inflammatory pain, with an easily understood relationship between the peripheral disease and degree of pain.
At this point in the disease process, NSAIDs would be expected to be effective. However, in many cases, the ongoing nociceptive input into the nervous system, along with damage to nerve endings as a result of the peripheral disease process, result in changes in the CNS producing maladaptive pain. It is this maladaptive component that makes chronic pain recalcitrant to NSAID therapy and difficult to treat (Figure 2). – hence the search for novel, non-NSAID therapies that can be used with, or in place of, NSAIDs.
It is probable different neurobiological processes are responsible for the various components of chronic pain and a long-term idealistic goal would be to understand all the mechanisms contributing to pain in a specific patient and use this information to choose appropriate analgesics. While this is not possible, progress is being made in this area, with studies in humans testing the function of the endogenous analgesic mechanisms to predict response to analgesics (Yarnitsky et al, 2012; Edwards et al, 2016), so this may be an option in the future.

Despite information suggesting NSAID therapy can partially reverse central plasticity (Arendt-Nielsen et al, 2016), it is generally accepted the maladaptive component of chronic pain conditions is poorly responsive to NSAIDs (Edwards et al, 2016).
Partly because of this, and due to concerns regarding potential adverse effects from NSAIDs, considerable interest exists in alternative drug therapies. Unfortunately, a paucity of peer-reviewed evidence is available in veterinary literature regarding these alternative therapies and most drug choices are based on experience in people, or because of their activity on mechanisms shown to be important in rodent models of maladaptive pain.
Medications suggested for the treatment of maladaptive pain associated with OA include gabapentin, tramadol, amantadine, amitriptyline, tapentadol, flupirtine and anti-nerve growth factor antibodies. Many of these have been discussed in Veterinary Times 2016 articles (Perry, 2016a;b) and this article will concentrate on those not reviewed previously or where evidence has become available since.
Tramadol is an opioid-like drug that exerts its effects via many different mechanisms of action, including very weak μ-opioid effects, norepinephrine and serotonin reuptake inhibition, and binding of α2 adrenergic receptors in the pain pathway (Raffa et al, 1992; Faron-Gorecka et al, 2004).
Significant species differences exist in the uptake and metabolism of tramadol; for example, dogs produce very little O-desmethyltramadol M1 metabolite after administration of tramadol – this is an active metabolite required for the opioid actions of this drug (Kogel et al, 2014). Cats, however, produce high concentrations of the M1 metabolite with resultant opioid and analgesic effects (KuKanich, 2013). As would be expected, the efficacy of tramadol appears to differ between cats and dogs with OA based on recent studies (Monteiro et al, 2016; 2017; Budsberg et al, 2018).
Two studies evaluated the efficacy of tramadol, either alone, or in combination with meloxicam, in research of cats with naturally occurring chronic OA-associated pain (Monteiro et al, 2016; 2017). Outcome measures used in these studies included kinetic gait analysis, whereby peak vertical force was measured, accelerometer-based motor activity and response to mechanical temporal summation. While larger studies in client-owned cats would be ideal, these initial studies, in addition to pharmacokinetic data, indicate tramadol may be effective in treating the maladaptive components of chronic OA-associated pain in cats (Figure 3).
Mydriasis, sedation, hypersalivation, vomiting and stomatorrhagia were observed in cats receiving tramadol (Monteiro et al, 2016; 2017) and it is suspected the medication’s bitter taste is responsible for the latter observations. Aversion to administration of this medication may present a clinical problem and compounding or reformulation may be necessary to resolve it.
In contrast, another study (Budsberg et al, 2018) evaluated the use of tramadol for treatment of pain and joint dysfunction in dogs with chronic OA. Outcome measures included kinetic gait analysis (with peak vertical force and vertical impulse being measured) and the Canine Brief Pain Inventory (CBPI). This was a randomised, blind placebo-controlled crossover study. A total of 35 dogs with stifle or elbow OA completed the study, receiving 10 days of tramadol at a dose of 5mg/kg every 8 hours, but no evidence was found the tramadol provided any clinical benefit for the dogs concerned. A significant improvement in the same cohort of dogs was noted when carprofen was administered.
The authors concluded their study provided no support for the use of tramadol in dogs with OA of the elbow and stifle joints, and they believe it is highly likely their findings can be generalised to other joints in dogs with OA. Considering the administration of tramadol is associated with some risk, including the development of serotonin syndrome (KuKanich, 2013), and given the lack of evidence supporting use of tramadol in dogs, the author recommends the use of alternative options for management of chronic OA-related pain in this species.

The centrally acting analgesic tapentadol, was developed to improve the therapeutic range of opioids by adding a different, complementary mode of action. It combines μ-opioid receptor (MOR) agonism and noradrenaline reuptake inhibition (NRI), and has been proposed as the first representative of a new class of drugs: MOR-NRI (Kress, 2010).
The MOR mechanism interrupts presynaptic and postsynaptic transmissions of ascending pain signals in the spinal cord and supraspinally activates the descending inhibitory projections (Tzschentke et al, 2014). It is primarily effective against moderate-to-severe acute pain. NRI increases noradrenaline concentrations in the synaptic cleft and enhances the body’s pain inhibition in the descending pathways. NRI drugs are particularly useful in chronic neuropathic pain conditions (Tzschentke et al, 2014).
As both mechanisms contribute to the analgesic effect, the inclusion of NRI reduces the “opioid load” and might ameliorate side effects associated with opioid use (Tzschentke et al, 2007). Synergistic interaction regarding analgesia between the two modes of action allows for strong analgesic effects despite the relatively moderate activity at the two target sites. The dual mode of action indicates suitability for a broad range of pain conditions – in particular, whenever a neuropathic pain component cannot be excluded (Baron et al, 2017). This makes it an attractive option for OA management.
A study evaluating the use of oral tapentadol in people with chronic knee pain due to OA demonstrated tapentadol provided superior pain relief and an improved overall health status when compared to oxycodone in a large patient population with moderate-to-severe pain. Tapentadol also showed a more favourable tolerability profile than oxycodone in this study (Lange et al, 2017). Prolonged release tapentadol has been available on the human market for six years.
A panel of specialists reviewed its role in the management of chronic pain (Baron et al, 2017), concluding tapentadol was an effective and generally well-tolerated treatment for up to two years in a broad range of chronic pain conditions, including those with neuropathic pain components.
Multiple studies have shown pain relief is at least comparable to that provided by controlled release oxycodone and prolonged release oxycodone/naloxone. Rotation from poorly tolerated opioids to tapentadol in people showed effective pain relief and better symptom control for musculoskeletal pain when compared to the previous medication. Functionality, health status and quality of life also improved under tapentadol treatment. The safety profile is good and no evidence of acquired tolerance from the long-term data has been collected so far. Overall, the review concluded tapentadol represented an effective and generally well-tolerated alternative to classical opioidergic drugs (Baron et al, 2017).
Information regarding use of tapentadol in domestic species is limited to date. Bioavailability following IV, IM and SC administration has been shown to be high in domestic species with a terminal half-life between two to three hours, depending on the route of administration (Lee et al, 2013). Side effects in cats and dogs include salivation and panting, with cats also showing agitation occasionally as is typical with opioid administration. Oral tapentadol has been shown to have a significant effect on skin thermal thresholds at one and one-to-two hours in cats when compared to the baseline (Doodnaught et al, 2017).
More information is required on the use of tapentadol in domestic species, including oral pharmacokinetics and evidence of analgesic efficacy; however, this does appear to offer a promising addition in the treatment of OA.
Flupirtine is an aminopyridine drug classified as a selective neuronal potassium channel opener (Devulder, 2010; De Vito et al, 2014). The mechanism of action is via interaction with G-protein-regulated, inwardly rectifying K+ channels (GIRKs), a class of potassium channel separate from the voltage-gated family.
GIRK channels contribute to the maintenance of resting membrane potential and manage the excitability of the cell. The activation of GIRK channels results in hyperpolarisation of the neuronal membrane and, therefore, flupirtine stabilises the membrane potential indirectly by activating GIRK channels, hereby decreasing neuronal excitability. Flupirtine also displays indirect NMDA receptor antagonism via the activation of potassium channels (Devulder, 2010; De Vito et al, 2016). Flupirtine has historical use for a range of conditions in humans, including chronic pain, migraines, musculoskeletal back pain, myofascial pain and postoperative pain (Devulder 2010; Harish et al, 2012). Opioid-sparing effects have also been demonstrated.
A study (Goswami et al, 2018) evaluated the efficacy and safety of flupirtine in primary knee OA in comparison to tramadol in people and concluded the effectiveness was comparable, while causing minimal adverse effects. This study only extended 12 weeks; therefore, the long-term benefits of the drug still needs to be explored. While flupirtine appears to be devoid of the adverse effects of NSAIDs and opioids, unfortunately acute liver hepatotoxicity (requiring transplant in some cases) has been reported in humans (Douros et al, 2013).
The bioavailability and half-life of the drug has been measured in cats following single doses at 5mg/kg both IV and PO (De Vito et al, 2014). The bioavailability was 39.3 +/- 9.7% after oral administration and the elimination half-life was 13.67 +/- 4.43 hours.
Data exists supporting efficacy of the drug in an electrical tooth pulp model in dogs and cats (Gordon et al, 1987; Nickel 1987), but the remaining evidence in animals is limited to non-companion animal models, including efficacy in rodent pain models (Kolosov et al, 2012). Further evaluation of flupirtine is warranted – the novel mechanism of action makes it an attractive option for multimodal management of OA, but lacks sufficient evidence to make treatment recommendations at this time.
Another drug being considered as a potential option for treatment of OA and other chronic pain conditions is maropitant. Maropitant is a potent and selective neurokinin-1 receptor (NK-1R) antagonist that functions as a central and peripheral antiemetic (Hickman et al, 2008). This receptor is also shared by the ligand substance P (SP), which has been studied for its role in inflammatory and nociceptive pathways (O’Connor et al, 2004).
Due to the knowledge that maropitant may have NK-1 antagonist activity, the known role of SP/NK-1 in pain, and the fact maropitant is approved for use in veterinary species, interest in evaluating the drug for analgesic effects has been sparked (Adrian et al, 2017). The anaesthetic-sparing effects of IV maropitant have been evaluated in cats (Niyom et al, 2013) and dogs (Boscan et al, 2011), and a significant anaesthetic sparing effect was noted in both species. The anaesthetic sparing effect appears to be greater in dogs, where the minimum alveolar concentration of sevoflurane was decreased by 24% to 30% (Boscan et al, 2011), where in cats the reduction was 15% to 17% (Niyom et al, 2013).
Additionally, another study demonstrated no major differences in cardiorespiratory parameters or anaesthetic requirements between maropitant and morphine when used as a pre-anaesthetic agent for ovariohysterectomy (Marquez et al, 2015). The explanation for maropitant’s effect in decreasing anaesthetic requirements during visceral noxious stimulation remains unknown. It is important to note, however, an anaesthetic sparing effect does not necessarily translate into effective analgesia, as has been demonstrated with midazolam (Seddighi et al, 2011). While initial pharmacological data are available, efficacy data are required before recommendations can be made for analgesia.
Another novel treatment for OA-related pain starting to appear in the veterinary literature is the use of mesotherapy. Mesotherapy is a technique used to inject active substances into the superficial layer of the skin (Pistor, 1976; Dalloz-Bourguignon, 1979; Rohrich, 2005). It consists of a series of microinjections of drug/active substance into the dermis using short needles.
Intradermal injection is proposed to allow slow diffusion of the drug into the tissues underlying the site of injection achieving higher concentrations in skin, muscle and joints corresponding to the site of injection than following IM injections. Mesotherapy is postulated to allow drugs to exhibit direct and prolonged local pharmacological activity (Pistor, 1976).
The objective of this type of administration is to modulate the pharmacokinetics of the injected substance and prolong the pharmacological effects at a local level. One of the main proposed advantages of mesotherapy is a local pharmacological effect can be obtained without the need for high systemic concentrations (Mammucari et al, 2011).
In people it has been demonstrated intradermal injections of small amounts of active substance where the injection site corresponds to the area of the pathological condition – for example in lower back pain – may provide clinical benefits where other therapies are not available/not effective or cannot be used for whatever reason (Mammucari et al, 2011). In addition, intradermal administration of active substances, in combination with other systemic therapies, can produce synergistic effects, and, as a result, mesotherapy may have dose-sparing effects (Mammucari et al, 2011).
Mesotherapy has been proposed as an acceptable alternative to the use of systemic NSAIDs in human patients with chronic musculoskeletal pain (Crosby, 2009; Mason et al, 2004). In one study evaluating the effectiveness and safety of mesotherapy (using lidocaine, piroxicam and calcitonin) and comparing this to the use of NSAIDs (diclofenac) in patients with knee OA, pain scores were improved in both groups of patients, but physical function was reported to improve more substantially in patients receiving mesotherapy (Chen et al, 2018).
Mesotherapy (using lidocaine, piroxicam and pentoxifylline) has also been reported to be effective for the treatment of temporomandibular joint disorders in people (Cruz et al, 2015). The number of randomised, controlled trials evaluating this treatment is low, and more investigation is needed to demonstrate efficacy and to provide guidance on what drugs/active substances should be used to allow the best effects to be obtained with the lowest risk of adverse effects. The results available in the human literature to date indicate this technique may provide clinical benefits and it is generally well tolerated.
Veterinary literature to date consists of one case report where mesotherapy using a combination of lidocaine, thiocolchicoside and piroxicam was used to treat a case of chronic elbow OA (Alves and Santos, 2017), and one small case series where mesotherapy using a combination of lidocaine, dexamethasone and thiocolchicoside was compared to the use of carprofen in dogs with chronic back pain (Alves et al, 2018).
Treatment success was reported for mesotherapy patients in both reports based on outcome measures, including the CBPI and Hudson Visual Analogue Scale, indicating mesotherapy may be a promising treatment option for canine musculoskeletal pain. However, further studies – preferably randomised controlled trials with larger case numbers and objective outcome measures – are necessary before treatment recommendations can be made.
Our understanding of the complex nature of OA-related pain is constantly increasing and we appreciate this pain consists of several different components, including an active sustained inflammatory component and maladaptive pain associated with neuronal changes and sensitisation.
In future, it may be possible to understand all of the mechanisms contributing to pain in a specific patient and use this information to choose appropriate analgesics. However, our increased understanding and recognition of these different types of pain can guide us in our therapeutic decision making and research endeavours in constantly seeking novel therapies to help us control all components of pain, while minimising adverse effects.