13 Jul 2022
Valentina Brioschi DipECVS, MRCVS outlines the most common issues afflicting this joint and provides a comprehensive insight into treatment.

Medial patellar luxation (MPL) is a developmental condition that most commonly affects small breed dogs; however, its incidence has been increasing in large breed dogs in recent years (Alam et al, 2007).
The aetiopathogenesis of the condition is not entirely understood. Various skeletal abnormalities have been reported to be associated with this condition, including malalignment of the quadriceps mechanism, coxa vara, coxa valga, distal femoral varus, shallow trochlear sulcus with poorly developed medial (and in some cases lateral) trochlear ridge, hypoplasia of the medial femoral condyle, medial displacement of the tibial tuberosity, internal rotation of the tibia relative to the femur, proximal tibial varus, proximal tibial valgus and internal rotation of the foot (Kowaleski et al, 2018).
In some cases, the patella can be difficult to find. In these cases, the clinician can palpate the patella ligament starting from its insertion on the tibial tuberosity and progressing proximally until the patella is located.
Repeated flexion/extension of the stifle with internal rotation of the tibia, and/or while applying medial and lateral pressure to the patella, allows to establish the grade (Table 1) and direction of the luxation.

Cranial drawer and tibial compression tests must be performed to assess for the presence of concomitant cranial cruciate ligament rupture.
Gait evaluation at a walk and trot is performed to assess the patient for the presence of obvious skeletal deformities, and to determine the severity and type of lameness. The degree of lameness can vary in dogs with MPL. Patients can be sound, they can present with an intermittent skipping lameness or, in very severe cases, they can present with a crouched gait with hyperflexion of the stifle joints.
In dogs with low grade MPL, orthogonal radiographic views of the stifle (usually tibial plateau levelling osteotomy [TPLO] views with the stifle and talocrural joints flexed to 90° on the mediolateral projection, as well as a straight caudocranial view of the stifle) are performed to assess the degree of degenerative joint disease (DJD).
In dogs undergoing tibial tuberosity transposition, the mediolateral projection can be used to plan for surgery (Figure 1).
In dogs affected by higher grades of MPL, or where skeletal deformities are suspected, orthogonal views of the femur and tibia or, alternatively, a CT study are needed to quantify the deformities present and plan surgical correction. CT is usually considered superior to radiography in accurately assessing bony deformities (Perry and Déjardin, 2021).
Skyline radiographic views of the femur have been described to assess the depth of the trochlear groove; however, they are rarely performed as they are difficult to obtain.
Furthermore, the depth of the femoral trochlea can be assessed by visual inspection during surgery.
Several factors must be considered when treating MPL in a dog.
Dogs affected by grade I MPL are usually asymptomatic and, therefore, surgical treatment is not indicated. Dogs affected by grade III and grade IV MPL are usually lame and, therefore, surgical treatment is recommended (Kowaleski et al, 2018).
Decision making in dogs affected by grade II MPL is more complex. Dogs with more severe or frequent lameness (such as daily episodes of lameness or numerous episodes of lameness across one month) are usually treated surgically, while dogs with occasional or no lameness are usually treated conservatively, and re-evaluated if lameness worsens.
A recent study estimated that approximately 50% of dogs with asymptomatic MPL will develop clinical lameness requiring surgical treatment within a four-year period (Hamilton et al, 2020).
The aim of surgery is to realign the quadriceps mechanism and improve congruity of the patellofemoral joint. Surgical treatment options for MPL can be divided into osteotomies and soft tissue procedures.

Trochleoplasty. The aim of trochleoplasty is to deepen the femoral trochlea to recess the patella and improve patellar stability. The procedure is performed in dogs that have a shallow trochlear sulcus.
The depth of the trochlear sulcus is assessed during surgery, and the decision on whether to perform a trochleoplasty is based on the surgeon’s subjective assessment and experience, as objective guidelines are not available.
As a general rule, most textbooks suggest the aim of trochleoplasty should be to recess the trochlea so at least 50% of the patella is located beneath the trochlear ridges (Kowaleski et al, 2018).
However, this recommendation is anecdotal and not based on clear scientific evidence.
Various trochleoplasty techniques and some modern alternatives have been described.
“Classic” trochleoplasty techniques include:
Trochlear block recession sulcoplasty (TBR): TBR achieves better recession of the proximal portion of the femoral trochlea compared to trochlear wedge recession sulcoplasty, providing greater resistance to patellar luxation with the stifle in extended position (Figure 2).
Trochlear wedge recession sulcoplasty (TWR): TWR is technically easier to perform compared to TBR, but provides less adequate recession of the proximal femoral trochlea.
Abrasion trochleoplasty: this technique involves deepening the trochlear groove by burring away the hyaline cartilage lining of the femoral trochlea and a few millimetres of subchondral bone.
It should only be performed in cases where severe loss of femoral trochlear cartilage, due to severe osteoarthritis, is present.
Trochlear chondroplasty: this technique involves elevating an articular cartilage flap and removing several millimetres of subchondral bone before replacing the flap. It can only be performed in young dogs (less than six months of age).
“New” trochleoplasty techniques, meanwhile, include:
Semi-cylindrical recession trochleoplasty: this is performed with a stainless steel bespoke hole saw (SCRT saw, New Generation Devices), with a diameter of 4mm to 18mm, in combination with a customised aiming guide. An advantage of the semi-cylindrical, rounded osteotomy is it is technically easier to perform compared to TBR, and carries a reduced risk of fracturing the femoral trochlear ridges and a reduced risk of fracturing the osteochondral block (Blackford-Winders et al, 2021).
Kite shield-shaped wedge recession trochleoplasty: this technique was described in a case series of seven dogs. The kite shield-shaped wedge is a modified osteochondral trochlear wedge in the shape of a wedge distally and of a block proximally. The aim is to offer improved proximal trochlear recession compared to a traditional TWR (Katayama et al, 2016).
Medial ridge elevation wedge trochleoplasty: This is a technique described in five dogs with hypoplastic medial trochlear ridge. It involves creating an asymmetrical osteochondral wedge, rotating it 180° and placing it into the recess, creating an elevated medial trochlear ridge (Fujii et al, 2013).
Alternatives to trochleoplasty techniques include:
RidgeStop (Orthomed, Huddersfield): this is an ultra-high-molecular-weight polyethylene curvilinear implant secured with three standard cortical screws that can be used to augment the medial trochlear ridge (Figure 3).
The implant has been designed to be used instead of a traditional trochleoplasty. An abstract describing 17 cases treated with this novel surgical implant was presented at the European College of Veterinary Studies Congress in 2014; however, outcome and complication rate for the procedure have never been reported in the peer-reviewed literature.
Patellar groove replacement (PGR; KYON, Zurich): this is a titanium prosthesis made of a base plate and a groove component (Figure 4). A single publication (Dokic et al, 2015) reported its use in 35 dogs affected by patellar luxation with severe femoropatellar osteoarthritis.

In this study, six dogs out of 35 (17%) experienced complications. Although infection was not a reported complication, the occurrence of infection is always a concern when prostheses are used. If infection occurred and the implants should require removal, the limited surgical options available for revision is a cause of concern when considering this technique (Perry and Déjardin, 2021).
Tibial tuberosity transposition. The decision whether tibial tuberosity transposition (TTT) surgery should be performed or not is based on visual assessment of the direction of pull of the quadriceps muscle. This is best performed with the patient anaesthetised and after the hair has been clipped for surgery.
The patient is placed in dorsal recumbency and the surgeon stands at the end of the table near the patient’s pelvic limbs, holding the pes. With the hip, stifle and hock placed in a neutral position, the direction of the patellar ligament is observed: if it is not parallel to the trochlear groove, then a TTT is recommended (Figure 5). The amount of transposition needed is based on the surgeon’s judgement.
The size of the osteotomy is planned on mediolateral preoperative radiographs of the tibia (Figure 1). Several methods have been recommended for fixation of the osteotomised tibial tuberosity. The most common method consists of double k-wire fixation with a figure-of-eight tension band wire (Kowaleski et al, 2018; Figure 6).
If possible, the distal periosteal attachment of the osteotomised tibial tuberosity should be preserved, as this has been shown to reduce the risk of implant-related complications (Rossanese et al, 2019). The recommended direction of insertion of the k-wires is caudomedial and slightly distal.
K-wires directed distally at a steep angle are at increased risk of loosening and should be avoided (Cashmore et al, 2014).
Anecdotally, it has been recommended to place the k-wires at the point of Sharpey’s fibres insertion, just above the visible curvilinear area that is the distal attachment of the patellar ligament (also known as the “smiley face”). This is because k-wires placed distal to the insertion of the patellar ligament could act as a stress riser and increase the risk of tibial tuberosity fracture.

This is not supported by scientific evidence, but it seems prudent to follow this rule unless contrary evidence is available.
Distal femoral osteotomy. Distal femoral osteotomy (DFO) is performed when significant limb deformity (such as distal femoral varus with or without femoral torsion) is present. Case selection for corrective osteotomy is controversial and in most reports is based on the author’s experience rather than scientific evidence (Perry and Déjardin, 2021).
In a recent report, patients with a preoperative anatomic lateral distal femoral angle (aLDFA) 8° to 10° greater than the reported breed-specific normal value were corrected to the breed-specific normal angle, or a target angle of 94° if the breed-specific value was not available.
Torsion correction was performed at the discretion of the operating surgeon to increase the femoral torsion angle to a target value of approximately 27° (Brower et al, 2017).
The corrective surgery usually consists of a lateral closing wedge osteotomy stabilised with a dynamic compression plate, supracondylar plate or locking DFO plate (Perry and Déjardin, 2021).
Soft tissue procedures have to be performed in combination with osteotomy procedures and cannot be used as the sole treatment for MPL. The most commonly performed soft tissue procedures consist of medial release and lateral imbrication of the joint capsule/retinacular tissue.
The diagnosis of cranial cruciate ligament (CCL) rupture is based on the demonstration of cranial drawer movement or a positive tibial compression test. Radiographs typically show osteophytes around the distal pole of the patella, fabellae, and tibial and femoral margins. Radiographs also show stifle effusion that is identified as effacement of the infra-patellar fat pad just cranial to the joint and caudal displacement of the fascial planes caudal to the joint (Figure 7).
Non-invasive advanced imaging of the stifle (through ultrasonography, MRI and CT arthrography) has been reported in dogs with a suspected CCL tear with no palpable stifle instability, or in cases were preoperative evaluation of the menisci was sought (Blond et al, 2008; Mahn et al, 2005; Tivers et al, 2008).
However, advanced imaging techniques are rarely used in clinical practice as they are not always readily available, due to the need for specialised equipment and trained personnel. Furthermore, they are also operator dependent and expensive.
Usually, meniscal inspection is performed via arthroscopy or arthrotomy. In dogs with a suspected CCL tear and stable stifle, the CCL is visually inspected via arthroscopy or arthrotomy after other stifle joint pathologies (including osteochondrosis of the stifle, immune-mediated polyarthropathy and other causes of stifle joint effusion) have been ruled out.
Arthroscopy is considered the gold standard technique for inspection and treatment of meniscal tears associated with CCL rupture. The improved illumination and magnification provided by arthroscopy allows more accurate inspection of the menisci (Figure 8). Recent studies have found arthroscopy is more accurate than arthrotomy in detecting meniscal tears – particularly when visual inspection of the menisci is performed in association with probing (Pozzi et al, 2008; Plesman et al, 2013). Probing was associated with increased sensitivity and specificity in detecting meniscal tears by arthrotomy as well.
However, arthroscopy requires specialised equipment, is more expensive and has a steep learning curve. For these reasons, arthrotomy is still widely used to detect and treat meniscal tears in dogs.
Treatment options for CCL rupture in dogs of any size consist of conservative management or surgical management. Surgical management is divided into intra-articular reconstruction, extracapsular stabilisation and osteotomy procedures. Intra-articular techniques have fallen out of favour, having been replaced by osteotomy techniques (Kowaleski et al, 2018).
Two historical publications report conservative management for treatment of CCL rupture. Case management consisted of strict rest for three to eight weeks and NSAIDs for 10 to 14 days, or intermittently when needed (Pond and Campbell, 1972; Vasseur, 1984).
Dogs were treated conservatively either because of mild instability and/or instability of less than four to eight weeks’ duration (Pond and Campbell, 1972), or because of concurrent medical problems and/or financial constraints (Vasseur, 1984).
Vasseur (1984) reported that 85% of small breed dogs undergoing conservative management had a good outcome against 20% of large breed dogs. The recovery period was four to five months for small breed dogs and six to seven months for large breed dogs.
Evaluation of limb function after treatment in this study was subjective and based on owner assessment. All dogs treated conservatively developed DJD and thickening of the stifle, and some dogs had a positive cranial drawer, despite the owner reporting a “good” outcome, leading the reader to doubt how good limb function actually was for these dogs.
No recent studies that have evaluated the outcome of conservative management in dogs affected by CCL rupture are available.
The use of stifle orthoses has been reported for conservative management of CCL rupture in medium and large breed dogs (Hart et al, 2016). In this report, 86% of owners were satisfied with outcome following use of orthoses to treat CCL rupture; however, 46% of owners in the orthoses group reported skin lesions associated with the device (Hart et al, 2016).
Rehabilitation has been shown to improve function in dogs after surgical treatment of CCL rupture (Monk et al, 2006; Au et al, 2010).
Although it is reasonable to assume that rehabilitation – as part of conservative management of CCL rupture – is likely to be beneficial, no studies have evaluated this.
Based on the experience of the author’s practice, they do not recommend conservative management in dogs affected by CCL rupture unless they are only very mildly lame, or in dogs that are not surgical candidates due to financial constraints or comorbidities.
Extracapsular stabilisation for CCL rupture in dogs was first reported by DeAngelis and Lau (1970). Subsequently, several variations of the technique have been described.
Extracapsular techniques involve the placement of a suture outside the joint capsule that spans the stifle joint, to mimic the function of the CCL in restraining cranial translation of the tibia with respect to the femur.
In other words, the cranial tibial thrust generated during weight bearing is resisted by the suture material.
The procedure is not uniform. The position of the suture attachment points, the method of attachment, and the type of suture vary from one modification of the technique to another (Kowaleski et al, 2018). A common feature to all of these techniques is that they rely on periarticular fibrosis for long-term stability, as the stability created by the suture is only temporary.
Ideally, suture attachment points would be isometric. Isometric points are two points (one located on the distal femur and one located on the proximal tibia) that remain equidistant throughout stifle joint range of motion and, therefore, represent optimal anchorage points for the extracapsular suture (Kowaleski et al, 2018).
Given the complex shape of the stifle joint and the lack of a centre of rotation, true isometric points do not exist. However, quasi-isometric points have been identified in medium and large breed dogs.
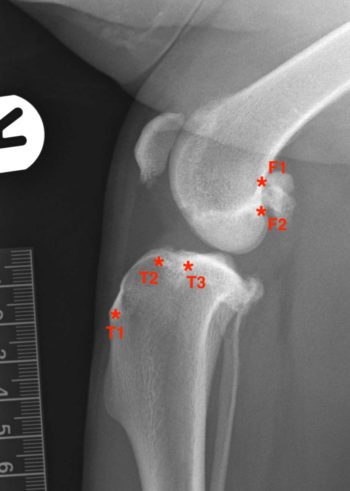
The preferred femoral attachment site has been reported to be F2 and the preferred tibial attachment site has been reported to be either T2 or T3 (Figure 9; Roe et al, 2008; Hulse et al, 2010). Examples of modifications of the lateral tibiofabellar suture reported in the literature include, among others: the Tightrope CCL technique (Arthrex), the SwiveLock bone anchor stabilisation (Arthrex), the Ruby Joint Stabilization System (KYON) and the LESS system (KYON).
Multiple studies have been published comparing the outcome for dogs undergoing TPLO surgery and extracapsular stabilisation. Bergh et al (2014) published a systematic review investigating which surgical procedure for the treatment of CCL disease has the best outcome.
They found that although the results of the studies published are often contradictory, taken together the evidence mostly shows TPLO as the procedure that allows dogs with CCL tears to return to normal function. In particular, functional recovery in the intermediate postoperative period is superior in dogs undergoing TPLO compared to dogs undergoing extracapsular stabilisation (Bergh et al, 2014).
The cranial closing wedge ostectomy (CCWO) technique was first described by Slocum and Devine (1984) to stabilise the CCL-deficient canine stifle.
Slocum and Devine (1983) described a force generated in the stifle during weight bearing created by the slope of the tibial plateau called the cranial tibial thrust (CTT). This force is normally counteracted by the intact CCL.
When the CCL fails, the CTT force causes cranial subluxation of the tibia relative to the femur during weight bearing. The aim of the CCWO was to eliminate CTT by levelling the tibial plateau and, therefore, providing functional stifle stability during the stance phase of the gait (Slocum and Devine, 1984).
The technique involves removing from the proximal tibia a cranially based wedge of bone distal to the most proximal point of the tibial tuberosity.
The aim is to achieve a postoperative tibial plateau angle (TPA) of approximately 6° (Warzee et al, 2001).
Multiple modifications of the technique have been described varying the position of the ostectomy in relation to the tibial tuberosity, the post-reduction alignment of the cranial or caudal cortices, the size and shape of the bone wedge and the method of fixation (locking or non-locking TPLO plates with or without pin and tension band wire; Figure 10).
Studies assessing the stability of the osteotomy, complication rate and outcome with different methods of osteotomy fixation have not been published and, therefore, the optimal method of fixation (Slocum-style TPLO locking or non-locking compression plate, with or without pin and figure-of-eight tension band wire) is not proven, although it is reasonable to assume a TPLO locking compression plate with cranial pin and tension band wire is most stable.
One of the downsides of CCWO surgery is that it causes shortening of the tibia; this gets worse the higher the TPA of the dog (Wallace et al, 2011).
The clinical significance of this is not known. Dogs are generally reported to have good function after surgery, but no studies have performed objective gait analysis in dogs that underwent CCWO surgery.
When performing CCWO surgery, one should also be aware that, depending on whether the osteotomy is positioned more proximally or distally on the tibia, and whether the cranial or caudal cortices are aligned after performing the osteotomy, a variation exists in the TPA achieved by the surgery (Bailey et al, 2007). The desired postoperative TPA is more likely to be achieved if the cranial cortices are aligned and the ostectomy is performed as proximally as possible.
However, given that the soft tissue tension doesn’t always allow to align the cranial cortices, accuracy in achieving the desired 6° TPA post-surgery is usually not possible and a degree of variation in postoperative TPA is to be expected.
TPLO was first reported by Slocum and Slocum (1993). The purpose of the procedure was, similarly to a CCWO, to eliminate CTT by levelling the tibial plateau and providing functional stifle stability during the stance phase of the gait.
This was achieved by performing a radial osteotomy centred over the intercondylar eminences of the tibia and rotating the proximal tibial plateau fragment to obtain the target TPA of approximately 6° (Slocum and Slocum 1993; Warzee et al, 2001; Figure 11). The procedure has become increasingly popular in medium and large breed dogs (Kowaleski et al, 2018), and it is slowly becoming more popular in small breed dogs in recent years (Brioschi and Arthurs, 2021).
As opposed to CCWO, accurate achievement of the target 6° postoperative TPA is usually possible with TPLO if the radial osteotomy is positioned accurately.
The original bone plate designed by Slocum to secure the osteotomised fragments was designed to accommodate three standard cortical screws in each fragment. Since the early 2000s, TPLO locking compression plates have become available and are currently sold by many manufacturers (Synthes, Arthrex and Veterinary Instrumentation among others).
The advantage of locking compression TPLO plates is that they better maintain tibial plateau position (as they allow less loss of reduction in the postoperative period), the locking screws are very unlikely to loosen and pull out in the soft metaphyseal bone of the tibial plateau, they need no or minimal contouring, and they provide greater construct stiffness and improved bone healing compared to non-locking plates (Kowaleski et al, 2013).
A systematic review investigating whether one surgical procedure is superior to the others when treating dogs with CCL disease found that, although mixed evidence exists in the literature, the evidence most strongly supports TPLO – rather than extracapsular stabilisation, CCWO and tibia tuberosity advancement (TTA) – as the procedure that allows dogs with unilateral CCL disease to return to normal clinical function (Bergh et al, 2014).
TTA was introduced for the surgical treatment of CCL rupture by Montavon et al (2002). The authors described an alternative biomechanical stifle model adopted from human medicine, where the direction and magnitude of the CTT is not determined by the slope of the tibial plateau (as described by Slocum and Devine, 1983), but by the “patellar tendon angle” (PTA), which is the angle between the patellar ligament and tibial plateau; a PTA greater than 90° generates CTT (Tepic et al, 2002).
Stabilisation of the stifle joint is achieved by performing a frontal plane tibial osteotomy, and cranially advancing the tibial tuberosity and the insertion of the patellar ligament to achieve a PTA equal to 90° at maximal stifle joint extension during weight bearing (Montavon et al, 2002).
In the “classic” TTA surgical procedure, stability of the tibial osteotomy is attained with a custom-designed tension-band plate and cage (KYON).
More recent modifications of the technique have eliminated the plate, and rely on the cage to provide advancement and stability of the tibia tuberosity.
Examples of these modifications of the original technique include the Modified Maquet Procedure (Orthomed), TTA Rapid (Rita Leibinger Medical), TTA-2 (KYON) and Fusion TTA (Fusion Implants).
Two recent studies have compared limb function after TPLO and TTA surgery. One study found that only dogs undergoing TPLO returned to normal function 6 to 12 months after surgery, while dogs undergoing TTA returned to normal function when walking, but not when trotting (Krotscheck et al, 2016).
Another study found that in the short term (two to three months after surgery) no significant difference was observed between dogs undergoing TPLO or TTA; however, dogs in this study were evaluated at a walk and not at a trot (Ferreira et al, 2016).
The triple tibial osteotomy (TTO) is a technique initially described by Bruce et al (2007).
The aim of the surgery is to eliminate CTT by reducing the tibial plateau slope to an angle perpendicular to the patellar ligament (as for TTA). This is achieved by making three osteotomies in the proximal tibia to create a partial cranial closing wedge ostectomy caudal to a partial tibial crest osteotomy.
Basically, the TTO technique combines features of both the TTA and CCWO techniques to achieve the same outcome, but with less radical angular changes.
The wedge ostectomy is stabilised with a TPLO plate and cancellous bone graft is packed at the site of the partial tibial crest osteotomy. Proposed advantages of TTO over other proximal tibial osteotomies include the need for less radical angular changes of the tibia than would be indicated in procedures that solely level the tibial plateau or advance the patellar tendon, minimal loss of tibial length, and minimal need for specialised surgical equipment or implants (Moles et al, 2009).
A paucity of reports exist on complication rate and outcome following TTO surgery. The postoperative complication rate has been reported to be 5% to 23% (Bruce et al, 2007; Moles et al, 2009), with tibial tuberosity fracture being the most common complication.
Only two studies reported long-term outcome assessed via an owner questionnaire. In both studies, the reported outcome was good (Bruce et al, 2007; Renwick et al, 2009). Biomechanical analysis of TTO and studies of long-term outcome of a large number of clinical cases have not yet been published.
Centre of rotation of angulation (CORA)-based levelling osteotomy (CBLO) is a procedure aimed at levelling the tibial plateau by aligning the proximal and distal anatomic axes of the tibia. The normal canine tibia has a proximal curvature (procurvatum) and, therefore, it has a CORA. When the proximal and distal tibial anatomical axes are drawn, the intersection of the two lines defines the position of the CORA. The angle formed at the intersection of the two axes determines the magnitude of the CORA.
When a CBLO is performed, the osteotomy is centred at the CORA, and the desired TPA is achieved by aligning the proximal and distal tibial anatomic axes.
The entire proximal tibial metaphysis is rotated. Proposed advantages of the technique are: preservation of the proximal tibial epiphysis to allow for application of an ancillary stabilising procedure if needed (that is, extracapsular suture); preservation of ample bone proximally for stabilisation, even in small breed dogs; and the osteotomy and implants are placed distal to the proximal tibial growth plate, allowing this technique to be performed in juvenile dogs (Kishi and Hulse, 2016; Raske et al, 2013).
The osteotomy is stabilised with a CBLO bone plate, locking screws and a headless compression screw. Studies of complication rate and long-term outcome of a large number of clinical cases have not yet been published.
The reported complication rate varies between 6% to 16% (Kishi and Hulse, 2016; Raske et al, 2013), with late meniscal tear being the most common complication in one report (Kishi and Hulse, 2016).
A study of 70 cases that investigated long-term outcome via an owner questionnaire found that outcome was good in 77% of cases, acceptable in 19% and unacceptable in 4%.