16 Apr 2018
Sarah Caney discusses effective ways of identifying this condition in cats and management strategies that can slow its progression.

Monitoring bodyweight can be a useful health indicator in cats. Most cats diagnosed with CKD will have lost weight in the one to three years preceding diagnosis.
Early diagnosis of chronic kidney disease (CKD) is desirable so appropriate treatment and monitoring can be implemented. Early diagnosis typically refers to diagnosis before the onset of clinical signs and requires proactive diagnostic testing.
A thorough history and physical examination is helpful in detecting subtle and non-specific signs of illness, such as weight loss, which may be seen in patients with CKD. Urine specific gravity testing is a simple and effective screening test for identifying patients that may be suffering from renal disease, and has the advantage of being possible in the absence of the cat. Blood tests, specifically creatinine and symmetric dimethylarginine levels, help confirm a diagnosis of CKD. Care should be taken to interpret blood creatinine and phosphate levels using International Renal Interest Society guidelines, rather than in-house or commercial laboratory reference ranges. Early diagnosis facilitates appropriate interventions with the potential to make a huge difference to both quality and length of life.
Optimum management of CKD includes transition to a therapeutic renal diet (where possible), symptomatic and supportive treatments, and consideration of medications that suppress the renin angiotensin aldosterone system. Attention to detail in patient assessment, good owner communication/support and regular check-ups improve long-term outlook.
Chronic kidney disease (CKD) is one of the most common causes of morbidity and mortality in older cats, estimated to affect more than 30% older than 10 years of age.
Unfortunately, a diagnosis of this illness is often only made following the appearance of clinical signs associated with azotaemia (raised urea and/or creatinine). By this stage, at least 75% of the renal function has been lost.
Diagnosis at an earlier stage is an advantage to the patient and owner, allowing earlier interventions and monitoring that help prolong life and aid quality of life.
Diagnosing CKD before the appearance of clinical signs is a challenge. To make an early diagnosis, attention should be taken to the following:
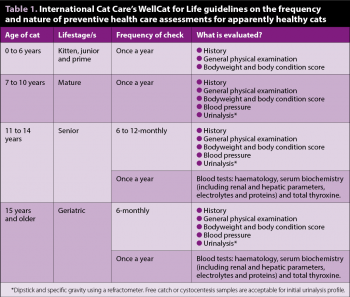
As older cats are more vulnerable to developing CKD, ”at-risk” patients should be targeted for assessment. The author recommends following International Cat Care’s WellCat for Life guidelines regarding the frequency and nature of diagnostic tests (Table 1).
Many clues of CKD are non-specific. Attention should be paid to looking for indicators of ill health, such as reduced appetite, increased thirst, weight loss, dehydration and abnormal renal palpation (such as microrenale, asymmetric kidneys, renomegaly, abnormal renal contours and pain).
It is important to note physical examination of patients with renal disease is often normal.
Weight loss is a valuable, although non-specific, indicator of ill health. Bodyweight and body condition score should be assessed on every occasion the cat visits the clinic. For cats older than 11 years of age, weight checks every three to six months are justified.
A publication reported a median weight loss of 8.9% bodyweight in the year preceding a diagnosis of CKD with weight loss evident as early as three years prior to the diagnosis being made (Freeman et al, 2016).
Renal disease is typically associated with a reduction in the ability to produce concentrated urine. For cats, this means a urine specific gravity (USG) below 1.035. Unless another reason exists for this ”low” USG, such as the cat receives a very liquid diet or enjoys drinking cat milk, further investigations are recommended.
Renal disease is not the sole cause of reduced USG – other common conditions that can cause it include hyperthyroidism and diabetes mellitus. Dipstick testing for glucose is helpful to rule out diabetes mellitus.

In cats where renal disease is confirmed, further urinalysis (ideally using a cystocentesis collected sample) is indicated. This should include a sediment examination, bacterial culture and protein estimation (urine protein to creatinine ratio; UPC) to further characterise the severity of disease and identify complications.
Free catch samples can be used for these further tests, but interpretation of results may be complicated by contamination from the urethra, genital tract and litter tray. The author considers a USG of 1.035 to 1.04 to be ”borderline”, with closer monitoring (for example, checking the cat again in three to six months) justified.
Many cats in early renal disease show few or no clinical signs. Blood screening allows the identification of azotaemia (raised urea and/or creatinine) in addition to looking for complications associated with renal disease, such as hyperphosphataemia, hypokalaemia and anaemia.
If possible, a symmetric dimethylarginine (SDMA) assay is an advantage.
SDMA is a renally excreted serum biomarker. Assessment of SDMA levels have been shown to be more sensitive than creatinine in facilitating an early diagnosis of CKD.
Unlike creatinine, SDMA levels are not affected by muscle mass, so this test may be more reliable in assessing renal function in a poorly muscled elderly cat (Braff et al, 2014; Hall et al, 2014).
Since the launch of SDMA, the International Renal Interest Society (IRIS) has updated its advice for clinicians:
Measurement of the glomerular filtration rate (GFR; the amount of blood passing through the glomeruli of the kidneys each minute) is considered to be the most reliable test of kidney function and commercially possible via the RVC using an iohexol clearance assay, although this is an expensive test to perform.
GFR assessment is not essential in all cases of CKD. It is most helpful when assessing cats with early kidney disease that are not yet azotaemic (such as IRIS stage one and early stage two CKD) and in screening cats known to be at risk of renal disease – for example, cats with congenital renal problems. Monitoring GFR test results over a period of time can be valuable in tracking progression of renal disease.
Blood pressure measurement is to be encouraged in all older cats, since systemic hypertension is a common entity in these patients. Cats with renal disease are especially vulnerable to developing systemic hypertension – between 20% to 40% of patients suffer from this potentially life-threatening complication.
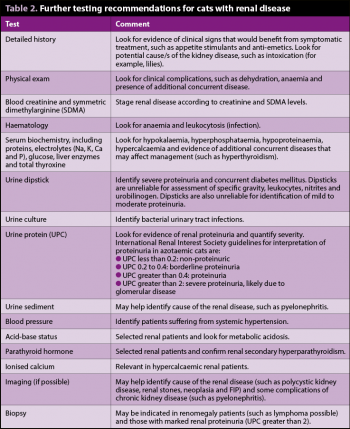
Further testing in confirmed cases of CKD is helpful in finding complications and learning more about the cause of the renal disease (Table 2).
Management of CKD should aim to:
Diagnosing underlying disease requires investigations, such as ultrasonography, urine culture and possibly other tests, such as biopsy, according to the individual’s needs. Unfortunately, in many CKD patients, the underlying cause of the disease cannot be identified.
The most proven general treatment for CKD is feeding a specially designed therapeutic renal diet (TRD). Studies have shown feeding a TRD improves quality and length of life of cats with CKD. TRDs are modified in a number of ways to support cats with CKD, with phosphate restriction considered the most important factor.
Phosphate restriction, through use of a TRD and/or phosphate binder, is effective in preventing/reversing renal secondary hyperparathyroidism and, hence, slowing progression of CKD. Acceptance of a TRD can take several weeks or months to achieve, and success depends on supporting carers through this period. Cats with CKD can be challenging to transition to a new diet and often require treatment for complications with a negative impact on appetite.
IRIS recommends phosphate restriction for all cats with azotaemic CKD (IRIS stages two, three and four), irrespective of their blood phosphate levels. If feeding a TRD is not possible then senior cat food is preferable to standard commercial cat food. Phosphate binders are useful if a TRD cannot be used, or if the TRD alone is insufficient to control serum phosphate.
Loss of nephrons leads to activation of the renin angiotensin aldosterone system (RAAS), which results in hypertrophy of residual nephrons with reduced arteriolar resistance and increased glomerular blood flow.
As renal disease progresses, the afferent arteriolar tone decreases more than the efferent arteriole tone, resulting in glomerular hypertension and hyperfiltration. Although this increase helps support GFR and excretory function; ultimately, RAAS activation has negative consequences, including proteinuria, renal damage, fibrosis and further progression of renal disease. Angiotensin II is responsible for many of the damaging effects of RAAS activation.
Assessment of renal proteinuria is helpful in judging whether RAAS activation is present in a patient. IRIS recommends CKD patients are classed as proteinuric if their UPC is greater than 0.4 and borderline proteinuric if their UPC is between 0.2 and 0.4. RAAS suppression using telmisartan or benazepril has been shown to be effective in reducing proteinuria, although a survival benefit has not been shown yet.
Some clinicians advocate treating borderline proteinuric cats (UPC 0.2 to 0.4) on the basis survival times in these cats are reduced compared to non-proteinuric CKD cats (UPC less than 0.2), and this is considered logical by the panel responsible for International Society of Feline Medicine consensus guidelines on diagnosis and management of CKD (Sparkes et al, 2016).
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) should only be used in clinically stable, normally hydrated cats. Treating non-proteinuric CKD patients with an ACE inhibitor or ARB may have some benefits, since studies have shown improved quality of life and a tendency for the renal disease to progress more slowly in these cats.
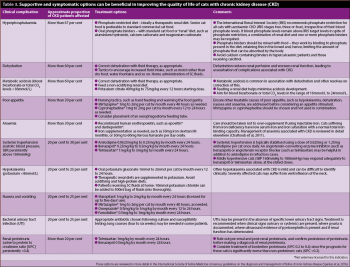
A variety of supportive and symptomatic treatments may be helpful in the individual patient, according to their needs, and summarised in Table 3. A successful outcome depends on an individualised approach, which is developed with involvement of the cat’s owner.
CKD is a complex disease and many owners appreciate support and education in how best to care for their cat. Monitoring visits are very important to ensure owners are supported, and clinical problems are identified and treated promptly. Compliance to medication and diet is enhanced by veterinary support – a study showed improved compliance to a TRD in those cats whose owners had received veterinary recommendation (Caney, 2017).
The required frequency of check-ups varies according to the patient’s needs, but should initially be at least once a month. Check-ups can be performed by a vet nurse/technician working under direction of a vet.
CKD is a common illness affecting at least a third of the elderly cat population. Diagnosis in the early stages is often ”hampered” by an absence of clinical signs; therefore, proactive steps are needed to identify patients suffering from this condition. Early diagnosis has the potential to be associated with a better patient outcome since it allows appropriate, targeted therapy at the earliest possible time point.
Since CKD is a progressive condition it is hoped early interventions will slow the progression of disease and help maintain quality of life. Once diagnosed, CKD can often be managed very successfully for several years. Attention to detail and providing an individualised plan leads to the best treatment outcome.