3 Dec 2021
Patrick Ridge details the diagnosis and treatment of a dog presenting with medial patella luxation and cruciate ligament failure.

A six-year-old, neutered, male terrier weighing 9kg was referred for investigation and management of a left hind weight-bearing lameness of a few weeks duration that had occurred suddenly after a slip.
On examination the left stifle was painful to flexion and the patella was medially luxated, but could be repositioned, although luxated spontaneously when the stifle was flexed. The stifle was also unstable to cranial drawer and tibial compression testing.

Under general anaesthesia a CT scan was performed of the hindlimbs from the pelvis to the toes and plain orthogonal radiographs were taken of the stifles to include the entire tibia. Measurements were taken from the CT of the anatomic lateral distal femoral angle (aLDFa) using the method described by Oxley et al (2013; Figure 1) and the tibial plateaux angle (TPA) was measured from the mediolateral radiograph using standard technique.
The results of the radiographic exam were as follows:
A diagnosis of cranial cruciate ligament (CCL) failure and concurrent grade three medial patella luxation (MPL) was given.
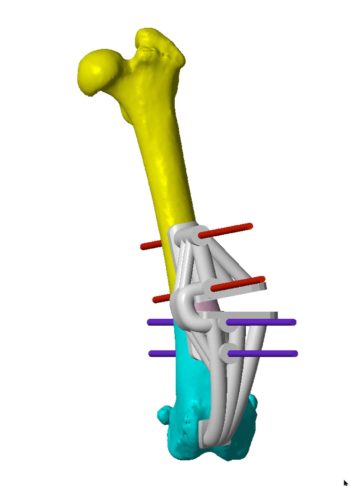
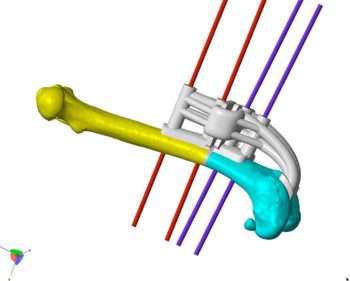
The CT scan data was sent to Vet 3D for assessment and planning of a distal femoral osteotomy (DFO). Using computer-aided design, Bill Oxley of Vet 3D planned a virtual DFO and created virtual guides to achieve this – these guides are designed to sit on the distodorsal femoral surface secured with 1.6mm Ellis pins. Reduction guides are then planned, secured with the same preplaced Ellis pins (Figures 2 and 3).
The guides are then printed in autoclavable, biocompatible resin along with a pre-op femoral model and a post-reduction femoral model. Implants can then be precontoured to the post-reduction model, therefore saving time during surgery and providing an extra level of confidence in robust fixation. During the fabrication period the dog was acclimatised to a cage to ensure close postoperative confinement.
Under general anaesthesia – with additional analgesia provided with morphine and meloxicam, and IV perioperative antibiotic cover with cefuroxime, a lateral parapatellar arthrotomy was performed and the distolateral femur approached.
Via the arthrotomy, with the patella luxated medially, the remnants of the CCL were removed, and the menisci checked and probed. A bucket handle tear of the medial meniscus was excised. The guides were then fitted to the distodorsal femoral surface and secured with 1.6mm Ellis pins.
Using the guides the DFO was performed, with the site lavaged copiously with saline. Once the DFO was complete the guide hinges were cut and the two parts of the guide were removed, leaving the pins in place. The DFO was then reduced and reduction was maintained using the reduction guide placed over the pre-placed Ellis pins. Accurate reduction was checked visually.
With the reduction guide in place the DFO was stabilised with the first precontoured lateral 2.0mm PAX plate (Securos) with 2.4mm screws distally and 2.0mm screws proximally. The reduction guide and Ellis pins were removed, and an additional 2mm PAX plate was placed on the dorsomedial aspect, with 2.0mm screws proximally and distally.
To free the patella medially the skin was retracted and the pes anserinus elevated from the proximomedial tibia. The adherent fibrous tissues fixing the patella were then carefully dissected from adjacent to the patella tendon proximally to the medial aspect of the femoral metaphysis. This medial release allowed the patella to return to the femoral sulcus without tension; normal patella tracking was checked and confirmed. A sulcoplasty was not performed.
Via the lateral approach the isometric points for stifle stabilisation were identified. The F2 location was confirmed just distal to the lateral fabella and as caudally as possible without entering the joint, and a mini guide pin was placed from the F2 location to exit the medial aspect of the distal femoral epiphysis.
Once placed and confirmed this was then over-drilled with a 2mm cannulated drill. The T3 location was identified on the tibia at the level of the joint surface just caudal to the sulcus of the long digital extensor tenon and another mini guide wire placed through the T3 location so that it exited on the proximomedial aspect of the tibia. Once confirmed in the correct location this was then also over-drilled with a cannulated 2.0mm drill bit.
Once all the tunnels were prepared, a length of 1.5mm suture tape (Arthrex) was passed around a 2.6mm oval titanium button (Arthrex) and the free ends were passed with a suture passing wire (Arthrex) from the medial aspect of the femoral tunnel to exit the F2 location on the lateral condyle.
The free ends were tensioned so that the 2.6mm button sat against the medial femoral cortex. The free ends were then passed through the tibial tunnel from the T3 location to exit the medial cortex and the free ends were tied over another 2.6mm button on the medial tibial cortex, therefore an isometric suture was placed to stabilise the craniocaudal instability and also address the internal tibial rotation caused by the cruciate ligament failure.
Stifle range of movement and stability were checked and confirmed, and patella tracking rechecked and confirmed. Finally the lateral capsule was closed and imbricated with three metric PDS, and the medial tibial approach and lateral femoral approach were closed routinely.
A postoperative CT confirmed the aLDFa to be 94 degrees and confirmed excellent osteotomy reduction, and robust implant purchase and fixation (Figures 4 to 6). Analgesia was continued for 24 hours with opiates and meloxicam continued for 3 weeks. Antibiotic cover continued for 10 days. The dog was confined to a cage for 6 weeks, having regular lead-controlled toilet walks. Skin sutures were removed after 14 days.
After 6 weeks on review he was walking comfortably and the patella was in place through a full range of movement. A small degree of tibial thrust existed on compression testing, but it was substantially less than pre-operatively.
Plain orthogonal radiographs confirmed stable implants and showed signs of union at the osteotomy site. Cage confinement was relaxed to house rest and the lead exercise was gradually built up over a period of 6 weeks. The dog’s owners reported full function at 12 weeks post-op and he was signed off.
Cranial cruciate rupture occurs as a result of a degenerative process that weakens the ligament gradually. The complete rupture may then occur as a result of only slight supra physiologic forces. The CCL stabilises the stifle in multiple planes, craniocaudal stability, prevention of hyper extension and also prevention of internal tibial rotation. In patients that have a predisposition to MPL the sudden loss of stability and especially the internal tibial rotation can acutely worsen the MPL as seen in this case.
MPL is caused by deviation of the quadriceps mechanism due to a skeletal abnormality. This can be due to femoral torsion, femoral varus, tibial torsion and/or medialisation of the tubercle. The femoral sulcus may also be shallow and secondary soft tissue changes develop with time, including lateral capsule stretching, and medial fibrosis and adhesions.
The use of CT in the pre-operative assessment of cases such as this allows for a very accurate assessment of femoral alignment and so helps determine the most appropriate technique to address the problem. Reluxation rates as high as eight per cent have been reported in the literature when addressing MPL in high grades using tibial tubercle transposition and sulcoplasty alone (Arthurs and Langley-Hobbs, 2006).
DFO is a very major surgical intervention, but the use of cutting and reduction guides makes the procedure substantially more accurate, and pre-operative implant contouring reduces surgical time.
In this case the small patient size would have made a traditional unguided surgery exceptionally challenging, not in the least that placing a jig may not have been possible, making osteotomy reduction and fixation challenging. Using locking implants biaxially as in this case provides a very robust fixation, but the author mandates cage confinement after a procedure such as this for all patients.
A number of different surgical approaches have been proposed to address both MPL and CCL rupture – these include tibial tubercle advancement with concurrent lateralisation, tibial tubercle transposition with isometric suture stabilisation and tibial plateau-levelling osteotomy (TPLO) with relative medialisation of the plateaux.
In this case, in the author’s opinion, the extent of femoral varus meant that to address the MPL a DFO was required. This could have been combined with a TPLO, but TPLO does not address internal tibial rotation, which we considered a major contributing factor to the MPL. Isometric suture stabilisation was therefore indicated.
The author has extensive experience in using the isometric suture technique, and the anchors and suture materials used – these materials require careful handling and scrupulous technique to avoid complications and maximise success.
The author would encourage surgeons interested in learning this technique to attend an official Arthrex practical course before embarking on this surgery.
This was a challenging case to address all the intimately-related causes of instability and the patient’s size added an additional level of complexity.
The use of cutting-edge technology with CAD allowed the author to plan in detail the procedure, and the use of miniaturised locking plate technology and robust yet small suture anchors allowed the surgeon to facilitate techniques used in larger patients in such a small complex patient.