4 Apr 2016
Ross Allan highlights signs, investigation strategies and therapy methods associated with a complication occasionally seen with neutering in canine and feline patients.

Figure 3a. In this cat, ovarian remnant syndrome was diagnosed and ovarian tissue found in the region of both the right and left ovarian pedicles.
Ovarian remnant syndrome (ORS) is a recognised complication of female dog and cat neutering. Recognising the symptoms and confidently diagnosing ORS is useful to review – especially as the symptoms may present many months, or indeed years, after the original surgery and with a large variation in severity and presentation.
Confident unequivocal diagnosis is essential prior to surgical investigation and management. Failure to adhere to this greatly increases the risk of disappointment and frustration, unlike the immensely rewarding experience successful ORS management offers.
As most cases originally occur due to veterinary surgeon error, swift, efficient diagnosis and successful treatment is likely to be beneficial and reassuring to all concerned – including the vets.
All vets in practice will recognise routine surgeries, such as ovariectomy (OVE) or ovariohysterectomy (OVH), may not always go to plan.

One recognised complication that can occur in both canine and feline OVE/OVH is ovarian remnant syndrome (ORS). This occurs due to failure to remove all of an ovary during OVE/OVH, ectopic ovarian tissue or auto-transplantation at the time of OVE/OVH (Ball et al, 2010).
The increased number of dogs rehomed across Europe and throughout the UK, with resultant registration at multiple practices, does, in the author’s opinion, increase the need to be aware of the signs to watch out for. Recognising the symptoms, confirming the diagnosis and managing appropriately is useful to review.
Often occurring in young, otherwise healthy, animals, managing ORS promptly and successfully is especially appreciated by owners and vets.
Taking a history is important in cases where ORS is suspected. Often, the behavioural and clinical signs noted by the owner greatly contribute to the diagnosis. However, a problem is the variation in the severity of the symptoms and how notable they are to the owner.
This makes taking a history, continuity of care and serial review important factors in reaching a diagnosis. Failure in any of these aspects is likely to prolong the time taken to reach a diagnosis.
While the experience of the surgeon performing the initial surgery may seem like a likely risk factor, other studies suggest this is not the case (Miller, 1995; Ball et al, 2010).
In dogs and cats, the symptoms that develop relate to the hormonal fluctuations that occur during pro-oestrus and oestrus. These symptoms may consist of vulvar swelling (Figure 1), serosanguinous to purulent vaginal discharge and mammary development. Behavioural symptoms may include attractiveness to males and postural behaviour (Naiman et al, 2014). Many animals will only have one or two of these symptoms.
It is recognised large variation exists in the time from OVE/OVH until the onset of clinical signs in dogs. One study described this as between 1 month to 120 months post-OVE/OVH, with a median of 17 months.
One factor important to consider is ORS may also occur in dogs with ovarian neoplasms. It is reported a longer gap can exist from OVE/OVH to ORS symptoms in dogs with ovarian tumours, 1 month to 60 months (median 12 months) in normal dogs, whereas in dogs with ovarian neoplasms, ORS was diagnosed 47 months to 120 months (median 96 months) post-OVH/OVE.
A variety of means may be used to confirm ORS, but all are conditional on first developing a clinical suspicion. In dogs where oestrus symptoms, such as willingness to stand, are apparent, the diagnosis can be simple and may only require vaginal cytology. However, other cases may have far less prominent symptoms and require more diagnostic investigation.
In dogs with a vaginal swelling, vaginal cytology offers a rapid and simple means of assessing whether oestrogen levels are elevated. The swab is taken in a similar way to when planning the time of mating, smeared on a slide and stained.
The presence of cornified anucleate or pyknotic vaginal epithelial cells confirms ovarian activity to be present. This, alongside clinical symptoms, may be the only step required prior to exploratory coeliotomy.
Abdominal ultrasonography can be used – especially in cases where ovarian tumour activity is suspected or where vaginal discharge occurs. Visualising the uterine stump will help assess whether there is enlargement or cystic change. In dogs, this is, itself, highly suggestive of ovarian activity. The reliability of ultrasonography to visualise and confidently identify an ovarian remnant issue will be greatly influenced by operator ability and this is likely a factor in the decision to perform blood samples.
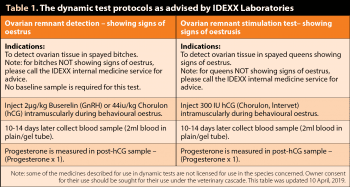
For both dogs and cats, two tests are routinely used to assess whether functional ovarian tissue is present. These are both stimulation tests using either human chorionic gonadotropin (hCG) or a gonadotropin-releasing hormone (GnRH) agonist to measure changes in progesterone or oestradiol, respectively (Idexx Laboratories, 2015; Table 1).
Key to performing the correct test is deciding whether the patient is exhibiting the actual signs of oestrus. hCG stimulation tests are performed if the patient does show signs of oestrus, while GnRH stimulation tests should be performed if the patient does not show any signs of oestrus.
This makes history and clinical assessment of the patient prior to blood sampling essential to optimising the chance of a correct diagnosis.
In one study describing 21 cases of ORS, performing only the vaginal cytology was required in 6 cases prior to exploratory coeliotomy. This contrasts with 5 animals that had 2 and 3 had all three diagnostic procedures (cytology, ultrasonography and hormonal analysis).

A further test has been shown to be highly effective at detecting ovarian activity in dogs and cats. This test detects anti-Müllerian hormone (AMH) – a protein hormone member of the transforming growth factor-β superfamily. In female dogs, the serum level of AMH markedly declines post-OVE/OVH as the ovaries are believed to be the sole source of AMH in the circulation.
The advantage of AMH assay over the previously listed tests is it is not a dynamic test and is, therefore, not reliant on the stage of the reproductive cycle (Place et al, 2011). This test has begun to be offered by UK commercial laboratories.
Exploratory surgery is required to visualise and remove the remaining ovarian tissue. A large coeliotomy incision should be made to allow full systematic examination of the entire abdominal cavity – even if, as in the author’s experience (and most cases described in the literature), the majority of ovarian tissue is found in the area of the ovarian pedicles (Figures 2a, 2b, 3a and 3b; Miller, 1995).
Some reports have suggested the surgery should be performed two weeks to four weeks post-oestrus as the luteal tissue may be more prominent and hence easier to locate (Hess, 2015). The author has not followed this and has operated when confident of the clinical evidence of ORS: irrespective of the stage of the reproductive cycle.
One study describes bilateral ovarian tissue in 10 per cent of ORS-affected animals and the presence of other ectopic ovarian tissue – either alone or in addition to this – cannot be discounted (Ball et al, 2010).

Enlarged uterine tissue, most often due to cystic endometrial hyperplasia, may also be seen at the time of surgery (Figure 4; Ball et al, 2010; Naiman et al, 2014). It is advisable to remove this tissue and submit it for histopathology. Stump pyometra secondary to ORS has also been described and, in cats, is described as resulting in severe disease and fatality.
Laparoscopic surgery has also been described for surgical management of ORS in dogs. Although palpating the tissues, which may be helpful in detecting ovarian tissue during surgery, is not possible to the same extent laparoscopically, the excellent visualisation of the ovarian pedicles can be helpful and in one paper, no cases required conversion to exploratory coeiliotomy to successfully treat ORS (Naiman et al, 2014).
All tissue removed at the time of surgery should be submitted for histopathology to ensure the ovarian tissue has indeed been removed and confirm whether any neoplastic tissue is present (Figures 5a, 5b, 6a and 6b).

While the presence of ectopic ovarian tissue is alluded to in a number of reports, specific reports of this occurring in dogs are difficult to find.
This, compounded by the published reports predominantly detecting ovarian tissue in the ovarian pedicle region, strongly suggests the vast majority of cases of ORS in dogs are due to surgeon error (Miller, 1995; Ball et al, 2010). These errors may be failure to remove all of the ovary or else inadvertent auto-transplantation of ovarian tissue during OVE/OVH.
This, along with the consideration that while accessory ovarian tissue has been reported in cats, cows and women, it has not, to the author’s knowledge, been detected in dogs and means ORS is, therefore, unfortunately most commonly due to human error.
The good news is ORS can be readily diagnosed if a full history is taken and the case followed up logically. While surgical management can be challenging, in the author’s experience, and the majority of published reports, locating the ovarian tissue is not as challenging as some textbooks may suggest (Miller, 1995; Ball et al, 2010).