12 Sept 2023
In the second of their two-part article, Chloe Fontaine and Renata Stavinohova discuss common pathogens causing this ocular condition, alongside the approach and management of cases.

Figure 1. Diffuse conjunctivitis associated with meibominan gland dysfunction (white upper conjunctival nodule) in a cat.
As discussed in part one of this article (VT53.15), conjunctivitis (Figure 1) is a common eye condition in dogs and cats. However, the causes differ depending on the species.
In dogs, the clinical signs of conjunctivitis are often caused by secondary bacterial infections such as Streptococcus and Staphylococcus or due to keratoconjunctivitis sicca. In cats, conjunctivitis is often caused by viral infections such as feline herpesvirus-1.
Clinical signs are similar to those seen in dogs and include chemosis (Figure 2), hyperaemia and discharge from the eye. Other symptoms include blepharospasm, discomfort and photophobia. However, in cats, if the discomfort persists and is not addressed, entropion and trichiasis will develop, contributing to corneal diseases (Figure 3).
Depending on the aetiology, ocular symptoms in cats may be accompanied by systemic symptoms such as respiratory signs and pyrexia.
Similar to what would be done with canine patients, cytology should be performed in every case of conjunctivitis. This can be performed with a cytobrush carefully rolled onto a microscope slide and stained with Diff-Quik. A swab of any ocular discharge can also be sampled and sent to the laboratory for culture. A snip biopsy of abnormal diffuse or localised conjunctival tissue can be submitted to histopathology (including specific stains and immunochemistry); this can aid in reaching a diagnosis.
Conjunctivitis in cats can have a variety of causes. Therefore, it is essential to have a thorough knowledge of the clinical signs and possible differential diagnoses to initiate the most appropriate treatment.
Anatomical differences between dogs and cats include the distribution of the mucous-producing conjunctival goblet cells. Dogs have a higher density around the lower nasal, middle fornix and lower tarsal portion of the palpebral conjunctiva. Cats, however, have a higher density on the anterior surface of the nictitating membrane and conjunctival fornices.
Like dogs, cats have a superficial adenoid layer containing lymphatic follicles (Figure 4) and a deep fibrous layer composed of nerves and vessels (Gelatt et al, 2021).

Viral infections are one of the most common causes of conjunctivitis in cats. Feline herpesvirus-1 (FHV-1) – a DNA virus and a member of the herpesvirus family – is the most common causative agent. The virus is shed in infected cats’ tears, saliva and nasal secretions, and can survive in the environment for several hours.
FHV-1 is a highly contagious virus that spreads through direct or indirect contact with infected cats or contaminated objects. Primary infection with FHV-1 causes ophthalmic and systemic symptoms such as pyrexia and respiratory symptoms. The cytopathic effect of the virus can lead to severely ulcerated conjunctiva, corneal ulceration with pathognomonic dendritic lesions and keratitis. FHV-1 is the only pathogen in cats known to initiate corneal ulcers, which can potentially become infected and lead to keratomalacia.

Corneal ulcers can lead to permanent lesions due to adhesions between tissues, called symblepharon (Figure 5), which can cause total blindness. Purulent nasal and ocular discharge is often the result of neutrophilic inflammation, even in the absence of secondary bacterial infection (Gould, 2011).
Ophthalmia neonatorum (Figure 6) can be caused by FHV-1 or other infectious (bacterial) agents in newborn kittens, and infection can also lead to symblepharon.

This condition is characterised by an accumulation of purulent material behind the eyelids before the resolution of physiologic ankyloblepharon (closed eyelids) disappears at 10 to 14 days of age. Surgical treatment should be carried out alongside topical broad-spectrum antibiotics and lacrimomimetics.
Once infected by FHV-1, the animal becomes a carrier; this occurs during acute replication of the virus within the epithelial cells, which then proceeds to ascend neural axons and reach the nucleus. The virus may become latent in the trigeminal ganglia, meaning no clinical disease exists. There, the virus only produces limited viral transcripts (latency-associated transcripts; LATs) and cannot be cultured (Maes, 2012).
Other PCR studies have also detected viral DNA in the cornea, optic nerve, conjunctiva, olfactory bulb, vestibular ganglia and autonomic ganglia of asymptomatic animals (Townsend et al, 2013). Recrudescence of the virus can cause unilateral or bilateral conjunctivitis that varies in severity (Figures 7 and 8). This may be triggered by a stressful event such as an illness, environmental changes or corticosteroid administration. Once re-activated, the virus follows the same descending neuronal sensory route to reach the peripheral epithelial tissues, otherwise known as the “round trip theory”.

As previously described, FHV-1 has a cytolytic phase, a latent phase and a “persistent phase”. This refers to a similar situation in the latent phases where the virus cannot be cultured; however, on top of LATs, other genes associated with low-grade inflammation are also expressed.
This phase would often be associated with more chronic non-ulcerative/immunologic disease forms, such as herpetic stromal keratitis, herpetic uveitis, lymphocytic conjunctivitis and possibly eosinophilic keratoconjunctivitis.
Finally, another mechanism may lead to metaherpetic disease. This results from anatomic changes secondary to cytolytic and/or immunologic disease. Clinically, this would result in symblepharon, tear film dysfunction secondary to goblet cell depletion, neurotrophic dry eye or corneal sequestra (Figures 9 and 10; Gelatt et al, 2021).
Vaccination against FHV-1 provides only limited and temporary immunity.
Diagnosis of conjunctivitis is made primarily by history, typical clinical signs and contact with other infected cats, as diagnostic tests are relatively insensitive. The PCR test is the most sensitive test for detecting viral DNA using Dacron swabs with plastic handles. Viraemia possibly occurs during primary infection, but not during recrudescence; PCR on blood is unnecessary. Positive results for FHV-1 DNA have been found even in clinically healthy cats, so treatment decisions should be made based on clinical signs.
Treatment of FHV-1 conjunctivitis in cats includes supportive care with topical antibiotics and lacrimomimetics. Antiviral medications may be prescribed depending on the phase of infection that the animal is undergoing. During the cytolytic phase, antivirals will be beneficial in reducing the severity and duration of illness by addressing rapid viral replication.
Antivirals alone are often ineffective during immunologic disease as the host’s immune response causes most clinical signs. Immunomodulatory therapy is therefore required.
In metaherpetic disease, antiviral or immunomodulatory therapies are unfortunately ineffective. No specific feline-developed viral therapy is available, as all medications have been developed for human herpes virus, but some have been tested and studied (Gelatt et al, 2021; Thomasy et al, 2011).
In the UK, ganciclovir 0.15% is the available topical ointment, which is administered until resolution of clinical signs. This medication appeared well tolerated and was effective against FHV-1 in vitro (Lewin et al, 2021). Oral famciclovir, demonstrating little toxicity in vitro, can also be used at reported doses ranging from 8mg/kg once daily to 140mg/kg three times daily. A three-times daily administration of 90mg/kg reduced clinical signs significantly in a study by Thomasy et al (2011).
Clients of infected cats should be made aware of the absence of veterinary-labelled treatment when deciding to use antivirals. However, it is sensible to consider this treatment in case of severe conjunctival disease; anecdotally, topical antiviral treatment is always commenced if FHV-1 is suspected.
Systemic antivirals should be used according to the case, given their potential side effects; they may be the only treatment to consider in cases that are not possible to medicate topically. Antivirals are virostatics and, therefore, require frequent topical application and no medication tapering to avoid resistance.
Feline calicivirus (FCV) is a less common viral pathogen that can cause conjunctivitis in cats. It is a non-enveloped RNA virus that primarily targets the respiratory tract causing nasal discharge, sneezing and oral ulcerations. Most cats recover spontaneously from ocular signs and do not require treatment; conjunctivitis caused by FCV without the presence of oral ulcers would be highly unlikely.
Diagnosis can be made based on RNA detection by PCR on blood, cutaneous scrapings or oral and conjunctival swabs. Topical antivirals are ineffective because their mechanisms of action target viral DNA replication and not RNA. Healthy cats should be vaccinated to protect them from upper respiratory disease; they can, however, still become infected (Gelatt et al, 2021).
Some bacteria are commonly associated with feline conjunctivitis, such as Chlamydia felis. C felis, an intra-cellular Gram-negative bacteria, can cause primary conjunctivitis in young cats (usually below five years old). The bacteria permanently infects respiratory, gastrointestinal and genito-urinary epithelial cells.
Clinical signs are often unilateral initially but may then spread to the second eye because of lytic cell damage during the release of C felis elementary bodies (Hillström et al, 2012).
Some cats can also exhibit upper respiratory clinical signs. Infection occurs via contact with contaminated ocular secretions or, less frequently, via aerosol. Co-infection with FHV-1 is uncommon.
Based on the presence of elementary bodies and basophilic inclusions in the cytoplasm of conjunctival epithelial cells on cytology, the diagnosis can be made. These can be seen from day three of infection, but decrease over the following two weeks and are less likely to appear in chronic cases, so this is not the most reliable diagnostic method (Gelatt et al, 2021).
PCR of a conjunctival smear, scrape or biopsy can also detect the DNA of the infectious agent and is the preferred diagnostic method. Culturing conjunctival swabs is a technically demanding process that can lead to false negatives if the organism’s viability is affected during transport or when the numbers of bacteria are low during chronic infection.
Oral doxycycline at 5mg/kg twice a day (or 10mg/kg once a day) for 28 days leads to local and systemic clearance of the organism. Especially in multi-cat households, treatment should be prolonged two weeks after the resolution of clinical signs. This should be followed by administering 2ml of fluid or food to prevent oesophageal strictures.
Topical tetracycline four times daily will improve clinical signs, but is not the only recommended treatment of choice. As per literature, chloramphenicol or fusidic acid are ineffective (Gelatt et al, 2021).
A live vaccine can attenuate clinical signs by decreasing replication, but does not prevent infection; this should be considered in a multi-cat household. Although the transmission rate from cat to human is low, it is a zoonotic disease, and owners should follow strict hand hygiene rules (Gelatt et al, 2021).
Another less common bacterial cause of conjunctivitis is Bordetella bronchiseptica – an aerobic Gram-negative bacteria that can cause sneezing, coughing, nasal discharge and conjunctivitis with ocular discharge. Dog and cat strains can infect both species, but cats are more likely to sneeze, whereas dogs will most commonly exhibit coughing.
Diagnosis is made by aerobic bacterial culture or PCR on nasal or oro-pharyngeal swabs. Nasal vaccination will lead to a positive PCR up to three weeks post-administration.
Serology is not the diagnostic method of choice due to the high rate of circulating antibodies in the feline population. Infection is often self-limiting, and the pathogen does not colonise the ocular surface. Treatment can therefore be limited to topical mucinomimetics (Gelatt et al, 2021).
Mycoplasma species – another bacteria – does not play a definite role in cat conjunctivitis. It has been isolated from healthy animals and described as commensal organisms from the feline conjunctiva and upper respiratory tract. However, it may thrive in an environment colonised by other pathogens, such as FHV-1 or C felis, or in young or immunocompromised animals (Sykes, 2014).
Clinical signs are non-specific and include the classic conjunctivitis triad of conjunctival chemosis, hyperaemia and serous to mucopurulent discharge. Cytology is an unreliable diagnostic method. Gram stains are inefficient, given the lack of cell walls of the bacteria.
Positive culture or PCR of conjunctival swabs are not necessarily clinically relevant. The treatment of choice is a three to four-week course of oral doxycycline, which would also cover a chlamydia infection. Topical tetracyclines can relieve ocular signs (Gelatt et al, 2021).
Mycobacterial conjunctivitis (Figure 11) was also reported and associated with granulomatous lesions (Stavinohova et al, 2019).
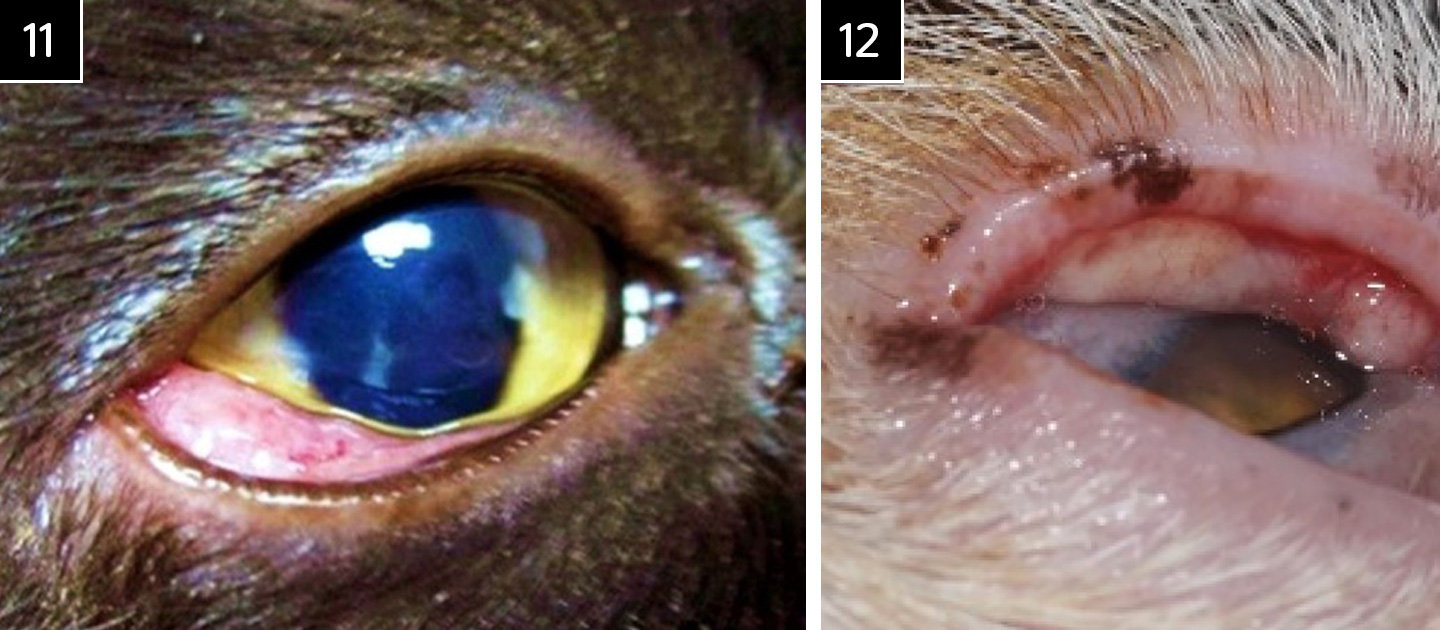
Lipogranulomatous conjunctivitis (Figure 12) can contribute to ocular irritation in cats. It is thought to be due to trauma to the meibomian glands, possibly due to sun exposure. The disease is characterised by white nodular lesions on the upper or lower lid margins bilaterally in middle-aged or older animals.
The typical clinical appearance and histopathologic findings of macrophages and multinucleated lipid-containing cells make the diagnosis. Surgical resection eliminates the clinical signs of blepharospasm and ocular discharge. Read and Lucas (2001) reported an absence of recurrence during a 4 to 21-month follow-up period after surgical treatment. Topical antibiotics were prescribed for seven days postoperatively.
Allergic conjunctivitis is a rare disease in cats. Clinical signs are similar to those seen in dogs with bilateral conjunctivitis, concurrent pruritus and skin lesions. The treatment of choice is the control of the atopy following a dermatologist’s recommendation and topical application of a steroid and lacrimomimetics (Gelatt et al, 2021).
Eosinophilic conjunctivitis is relatively common and may present symptoms similar to allergic conjunctivitis, excluding skin disease. This can affect the cornea (Figure 13) or be purely localised to the conjunctiva and/or free eyelid margin/eyelids (Figure 14). Cytology showing the presence of eosinophils and mast cells allows diagnosis (Figure 15).
The role of FHV-1 in this pathology remains uncertain, but should be considered (Labelle and Labelle, 2023). Treatment may be life-long and includes topical corticosteroid therapy or immunomodulators such as cilosporin A (Allgoewer et al, 2001).
Systemic steroids should be used with extreme caution if topical management is not possible. Megestrol acetate – an oral progestogen with glucocorticoid activity – has severe potential adverse effects due to adrenocortical suppression, but has been useful in treating severe disease rapidly (Gelatt et al, 2021). A topical formulation of megestrol acetate has also successfully been used to treat the condition (Stiles et al, 2016).
Systemic treatment with SC triamcinolone has also been proposed as management of the eosinophilic keratitis condition in cats (Lucyshyn, 2021).
The authors do not use megestrol acetate or systemic steroids given their severe potential adverse effects.
Epitheliotropic mastocytic conjunctivitis has similar clinical signs to those seen in animals affected by eosinophilic conjunctivitis, but often presents with more severe proliferative lesions – especially on the third eyelid. These lesions can sometimes be mistaken for squamous cell carcinoma.
The lesions are often unilateral, but can affect the animal bilaterally. Diagnosis is reached with characteristic histopathology lesions of intra-epithelial and sub-epithelial mast cells and with papillary epithelial hyperplasia. The treatment of choice is similar to what is used in eosinophilic conjunctivitis. Long-term management may be required as relapses are common (Beckwith-Cohen et al, 2017).
As in dogs, parasites can also affect the conjunctiva. These include Thelazia or Cuterebra. Treatment of Thelazia – a zoonotic disease transmitted by the fruit fly – has been successfully achieved with oral milbemycin oxime (2mg/kg) twice at a one-week interval, as well as with the manual removal of the parasite, which combined with topical antibiotics and anti-inflammatory agents may help relieve secondary clinical signs (Spoerel et al, 2020; Gelatt et al, 2021).
Neoplasms can irritate and contribute to conjunctivitis in cats. These include adenomas, adenocarcinomas, mast cell tumours, lymphomas, squamous cell carcinomas and melanomas. These tumours may arise from the palpebral, bulbar or fornix conjunctiva. Diagnosis is made by biopsies of the affected tissue and histopathologic analysis. Staging is essential, and sampling of locoregional lymph nodes (mandibular) is therefore advisable, as is thoracic imaging.
Treatment depends on the type and extent of the tumour. It may include surgical excision, radiation therapy, chemotherapy, or all. The prognosis depends on the type of neoplasm. For example, melanomas, although rare, have a higher metastatic rate than dogs (14%) and a high mortality rate of 61%, and recurrence is common despite surgical removal, even with enucleation.
Melanomas have a predilection for the bulbar conjunctiva (Payen et al, 2008). Conjunctival lymphomas are also rare in cats. Holt et al (2006) reported that chemotherapy did not improve lymphomas after removal. However, complete remission was achieved after radiotherapy.
Squamous cell carcinomas (Figures 16a and 16b) rarely affect the conjunctiva, but may invade adjacent tissues by the progression of eyelid neoplasia.

Similar to what was described in the canine patient, conjunctivitis can occur secondary to other ocular problems, such as adnexal diseases, abnormal cilia, caruncular trichiasis, entropion (Figures 17a and 17b), uveitis, ocular trauma or foreign bodies.

Keratoconjunctivitis sicca in cats is not as common as in dogs, but can occur and is usually either secondary to herpetic keratoconjunctivitis or can be secondary to radiotherapy.
In summary, conjunctivitis is a common ocular disease in cats caused by various factors, including bacterial or viral infections, lipogranulomatous conjunctivitis, eosinophilic conjunctivitis, parasites or neoplasms, or can develop secondary to other ocular problems.
Symptoms of conjunctivitis in cats still include the classic triad that also occurs in dogs. Intra-ocular, systemic or adnexal disease should be excluded to determine whether the conjunctivitis is primary or secondary.
Treatment depends on the underlying cause of the disease and may include antibiotics, antiviral medications, corticosteroids and supportive measures. Preventive measures such as vaccinations and good hygiene practices can also help manage these diseases.