20 May 2019
Ian Self discusses acute and chronic forms, assessment using recognised scales, and treatment option.

Dog exhibiting the “prayer position” typical of cranial abdominal or renal pain.
Pain has been defined by the International Association for the Study of Pain (IASP) as “an unpleasant sensory or emotional experience associated with actual or potential tissue damage, or described in terms of such damage” (IASP, 1994).
A more recent addition to the IASP’s definition has been: “The inability to communicate in no way negates the possibility that an individual is experiencing pain and is in need of appropriate pain-relieving treatment.” This shifts the onus on to veterinary professionals to realise that a patient who may be expected to be in pain (for example, following major surgery), yet is not necessarily demonstrating classical signs of pain, should be regarded as requiring analgesia.
An alternative definition attempting to define pain in animals is “an aversive sensory and emotional experience which elicits protective motor actions, results in learned avoidance and may modify species-specific traits of behaviour including social behaviour” (Morton et al, 2005). This is, arguably, a better working definition as it takes into account the altered behaviour commonly seen in animals experiencing pain, although the sensory and emotional components are still difficult to evaluate.

Acute pain is provoked by a specific disease or injury, serves a useful biologic purpose, is associated with skeletal muscle spasm and sympathetic nervous system activation, and is self-limiting (Grichnik and Ferrante, 1991). Acute pain is a necessary evolutionary trait allowing localisation of trauma/injury, plus the ability to gauge the likely severity of the inciting cause.
The definition of chronic pain has traditionally been based on time (typically between three to six months). However, perhaps a better definition would be pain extends beyond the expected period of healing. This indicates chronic pain is pathological in nature and serves no useful biological purpose.
Nevertheless, definitions are not always helpful to us as clinicians – for example, OA pain, which is chronic in nature, yet appropriate to the disease, especially during “flare ups”. In this case, it is appropriate to say OA pain is nociceptive (caused by inflamed or damaged tissue activating nociceptors), despite the chronic nature of the condition and that the pain is “appropriate” to the condition, whereas chronic (pathological) pain is neuropathic (caused by damage to or malfunction of the nervous system).
If we accept pain exists in animals the same as it does in humans, we should also ask if it has any useful functions and why we need to treat it.
Ethically, veterinary professionals have both a professional and moral duty of care to animals. On entering the profession, each UK vet takes an RCVS oath to “ensure the welfare of animals committed to my care”. In addition, most small animals are our companions and rely on us to protect their welfare, including their day-to-day requirements and freedom from pain. It has been argued animal pain is “worse” than human pain.
Animals are thought to live in the “now” and, unlike a human in pain, unlikely to be aware the pain is only temporary and will be relieved given time or treatment (Robertson, 2002).
As aforementioned, pain does serve a useful biological function in allowing us to locate and “deal with” an area of damage. However, once the cause of the pain has been identified and the underlying condition addressed, treated pain serves no further useful function and a number of well-recognised physiological consequences of untreated pain exist (Self and Grubb, 2019). These include:
It is also likely failure to manage acute (perioperative) pain may lead an animal to self-traumatise, potentially leading to the development of chronic (pathological) pain. Overall, these physiological changes associated with poorly controlled pain increase postoperative complications in surgical patients, as well as causing client dissatisfaction with the veterinary practice.
Regarding OA, 20% of adult dogs (Johnston, 1997) and more than 22% of adult cats (Bennett et al, 2012) demonstrate radiographic signs of degenerative joint disease. Effective management of pain in such conditions is imperative for the welfare of affected animals; dogs affected by OA have been identified as experiencing decreased quality of life, compared to unaffected dogs (Wiseman-Orr et al, 2006).
For years, veterinary professionals have been trying to predict how painful a condition is likely to be and treating accordingly. However, this approach takes little account of the massive variability seen in a patient’s response to a given painful stimulus. When applied prior to surgery, it could be said this approach is a pre-emptive pain scoring system, based on the science of the preservation of the pain pathway across mammalian species, with the addition of anthropomorphism, and the projection of human emotions and feelings on to animals. Obviously, not an ideal situation.
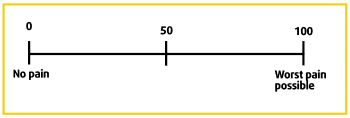
One of the most important breakthroughs in small animal pain medicine has been the introduction of validated pain scoring systems, which have allowed us to attempt to quantify acute pain and adjust analgesia accordingly, always bearing in mind companion animals that are expected to be in pain, but score low on pain scales, should always be given the “benefit of doubt” and analgesia should be administered. The author uses pain scales purely to monitor a patient’s response to analgesic therapy, adjusting doses/agents according to the changes in pain score over time.
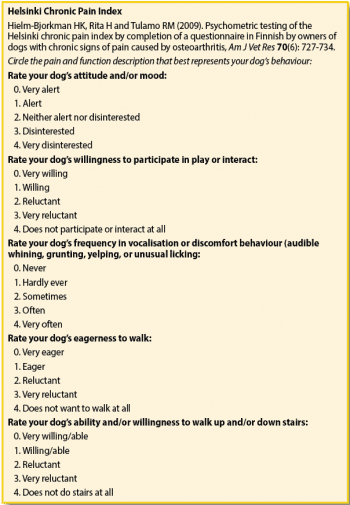
Unfortunately, no such “whole body” scales are validated for chronic pain in dogs. However, several validated scales do exist for assessment of OA pain (White and Hunt, 2019), including:
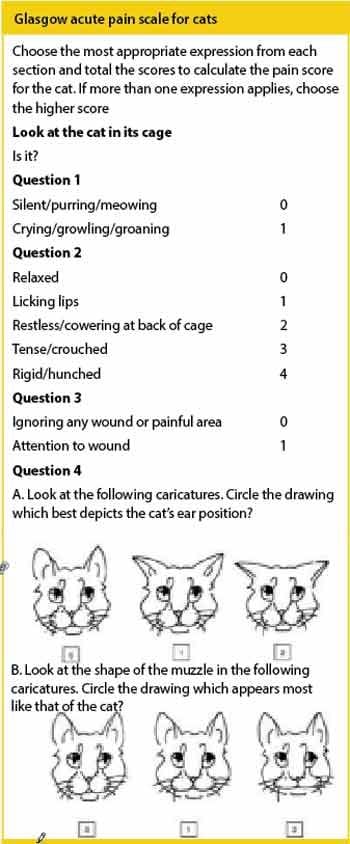
In cats, no universally accepted validated scale for OA pain exists, however, the following are examples of published scales:
Another major concept when dealing with chronic pain of any cause is quality of life or “suffering”.
Recognition is growing, as in human pain medicine, that while it is not always possible to fully eradicate pain, the emphasis should be on the impact of the pain on the individual’s daily life and allowing the patient to cope with its condition. To this end, validated quality of life scales, such as the online Vetmetrica HRQL system (https://bit.ly/2WrS3pn), are likely to become increasingly important when dealing with patients experiencing chronic pain.
Chronic pain may result from:
Initially, pain originates from nociceptive inputs (thermal, pressure or chemical) via activation of specific ion channels (for example, transient receptor potential vanilloid 1, transient receptor potential ankyrin 1 1) located on Aδ- and C-fibre nociceptor cell membranes, leading to the production of action potentials, which are transmitted to the dorsal horn of the spinal cord. Here, various receptors (mainly α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor; AMPA and N-methyl-D-aspartate; NMDA) are activated leading to projection to the brain stem, from where autonomic responses to nociception are coordinated, and transmission to higher centres allowing localisation of pain and appropriate behavioural responses to be made.
In some cases, such as ongoing inflammatory diseases, tissue damage liberates inflammatory molecules from damaged cells that maintain nociceptors in a state of hyperexcitability (producing hyperalgesia), and generation of spontaneous action potentials (causing spontaneous pain). Neuropathic pain arises as a direct consequence of lesions affecting the peripheral or CNS (Treede et al, 2008), such as spinal cord compressive disc lesions. This type of pain is not the same as central sensitisation (see later), which leads to the development of chronic (pathological) pain, but may contribute to such a state.
Central sensitisation may arise due to a number of mechanisms (White and Hunt, 2019):
Increased facilitation of nociceptive input due to repeated C-fibre stimulation activating the NMDA receptor. Also seen is postsynaptic facilitation due to release of substance P, tumour necrosis factor and prostaglandins. This contributes to the clinical phenomenon of hyperalgesia.
A failure of inhibitory interneuron activity permits sensations, such as touching or stroking of the skin (transmitted on Aβ fibres), to be misinterpreted as painful (allodynia; Sandkühler, 2009).
Reduced descending noxious inhibitory control (DNIC), a reflex that normally results in decreased dorsal horn activity in response to noxious stimuli. In OA, decreased efficacy of DNIC has been reported (Kosek and Ordeberg, 2000).
Glial cell activation – experimental inhibition of glial cells reduced the development of hyperalgesia in rats (Chacur et al, 2009). It is thought glial cells are important in “maintaining” painful states via facilitated transmission of nociceptive inputs.
The following treatment options are based on a study by White and Hunt (2019).
NSAIDs are the most commonly prescribed medications for treating chronic pain in dogs and cats, producing a peripheral anti-inflammatory effect, and can cause a reduced sensitisation within the CNS. Significant inter-patient variability in terms of efficacy and side effects exist. In animals that show a lack of response to one NSAID, it is worth considering swapping to another for an improved response, allowing a five to seven-day washout period between the drugs (KuKanich et al, 2012).
Paracetamol is widely used in human pain treatment, but no evidence exists to support the use of paracetamol in OA in dogs. Nevertheless, in the author’s experience, it appears to provide good, if variable, analgesia for chronic pain conditions when administered at appropriate doses. A licensed form of paracetamol that also contains codeine exists. Paracetamol should be avoided in cats.
Steroids can be of use if the chronic pain has an inflammatory component, but are not a commonly used first line treatment because of the side effects associated with long-term use. Similarly, long-term administration of opioids in cases of chronic pain is uncommon because of the side effects caused by these drugs, although they may be of use in a multimodal approach in cases of flare-ups.
Tramadol is an atypical synthetic opioid (KuKanich and Papich, 2004); however, a large variability in uptake exists and the author finds it has extremely limited efficacy in the treatment of chronic pain in dogs. It can be useful in cats, but the side effects, such as dysphoria and agitation, often mean treatment has to be withdrawn. Tramadol alone is unlikely to be efficacious for treating chronic pain.
Gabapentin has been successfully used as a first line treatment in animals with neuropathic pain (Grubb, 2010) and can be useful in managing chronic pain, especially in cats unable to tolerate long-term administration of NSAIDs (Robertson, 2008). Pregabalin is similar to gabapentin – both being structural analogues of gamma-aminobutyric acid.
Amantadine is a NMDA antagonist drug and can be used alone for treating chronic pain or in conjunction with NSAIDs in dogs with chronic OA pain refractory to NSAIDs alone (Lascelles et al, 2008). Although the most commonly recommended dose is 3mg/kg to 5mg/kg once a day, 2mg/kg to 10mg/kg two to three times daily has also been suggested (Pozzi et al, 2006).
Amitriptyline is a tricyclic antidepressant used in humans for controlling neuropathic pain, and one small study has documented its use in treating neuropathic pain in dogs at a dose of between 0.25mg/kg and 2mg/kg once a day to twice a day. It should not be used with tramadol or other drugs that inhibit serotonin and norepinephrine uptake.
In addition to pharmacological treatment, other management strategies need to be considered when dealing with chronic pain states, and the plan with OA pain should include analgesia, joint protection and nutritional support, as well as therapies such as physiotherapy, hydrotherapy and acupuncture, which play a large role in ensuring patient comfort.
Discussions with the owner should include environmental modification (ramps, eradication of slippery floor surfaces), enrichment, such as grooming, stroking and patting acting as a gentle form of massage, and an exploration of the various nutraceuticals available, of which the main evidence points to a benefit of oral supplementation with omega-3 fatty acids found in some fish oils and green-lipped mussel extracts (Roush et al, 2010; Bui and Bierer, 2001). It is also important owners address weight reduction in their pets; a moderate weight loss can reduce pain scores in animals suffering from OA (Marshall et al, 2010). Weight loss alone has been shown to improve quality of life in dogs (German et al, 2012). In addition, exercise has been shown to have a significant benefit in chronic pain conditions (Bobinski et al, 2015).
An increasing recognition exists of the need for robust treatment of pain. A 2013 survey showed almost ubiquitous use of analgesia for neutering cats and dogs (98% of respondents administering an NSAID; Hunt et al, 2015). This is in contrast to a 1996/1997 survey by Capner et al (1999) showing a much lower level of analgesic administration to cats and dogs undergoing routine neutering, with only 26% of cats receiving analgesia (Capner et al, 1999; Lascelles et al, 1999). Therefore, there seems to be significant improvement in the use of available analgesic agents, and further development in the delivery strategies of these drugs shows promise. For example, a liposome formulation of bupivacaine (local anaesthetic) administered as a single treatment into the tissue layers during surgical closure, which offers postoperative relief for up to 72 hours after surgery recently licensed in the US for dogs and cats. Interest has also been seen in sustained-release depot formulations of opioids such as buprenorphine, although none are, as yet, commercially available.
In addition to novel delivery strategies, some novel analgesics exist that are likely to become more readily available for companion animals. Intra-articular treatments for OA are of interest and aim to encourage healing of damaged tissue directly. Several agents have been examined, including autologous conditioned serum, platelet-rich plasma and cultured bone marrow-derived stem cells. Intra-articular introduction of adipose-derived stem cells has shown efficacy in canine OA for six months following injection (Black et al, 2007; Black et al, 2008). Early results are promising, but further clinical trials are necessary and none are yet at the commercially available stage.
Newly licensed in the UK for treatment of canine OA is grapiprant, a novel NSAID of the piprant class. Rather than decreasing prostaglandin formation by inhibiting the cyclo-oxygenase enzymes, grapiprant is a prostaglandin receptor antagonist, which antagonises the EP4 receptor, the primary mediator of canine OA pain (Kirkby Shaw et al, 2015), but does not interfere with homeostatic mechanisms mediated through other receptors.
Nerve growth factor (NGF) has been found to play a critical role in nociception and its upregulation in dogs’ and cats’ pain conditions. Two studies have been published demonstrating an analgesic effect of IV administration of a canine nerve growth factor antibody to dogs (Webster et al, 2014; Lascelles et al, 2015).
Some clinical work has been carried out examining the use of monoclonal antibody (mAb) therapies targeting chronic pain, and species-specific anti-NGF mAbs have been developed for the management of OA-associated pain in dogs and cats; early clinical trials show anti-NGF therapy appears very effective (Enomoto et al, 2019).
Finally, the benefits of a multi-disciplinary approach to pain treatment is being recognised with increasing numbers of clinics dedicated to the management of pain allowing integration with physiotherapy, hydrotherapy, nursing and complementary therapy teams.
The importance of chronic pain recognition, assessment and treatment is increasingly recognised in companion animal medicine. In no small part, this is due to increased knowledge about the detrimental effects of pain, improvements in communication to undergraduate and postgraduate veterinary professionals, increased numbers of licensed analgesic drugs and the introduction of validated pain scales. Interesting developments are planned in this field that will continue to benefit veterinary patients.