5 Feb 2021
Joy Ioannides BSc(Hons), BVetMed(Hons), PGDipVCP, MRCVS explores the categorisation, diagnosis and treatment of this condition that commonly causes blindness in dogs.

Figure 1. Distant direct ophthalmoscopy technique.
This article explores the categorisation, diagnosis and treatment of canine cataracts.
Cataract is an opacity of the lens or lens capsule. The opacities may vary in size, shape and location within the lens.
Transparency of the lens is imperative for vision; the transparency is maintained by a number of factors, including highly structured organisation of uniform lens fibres, a relative dehydrated state, a lack of intracellular organelles and a high percentage of soluble proteins. When any of these factors are altered, cataract forms, causing light to be scattered rather than passing uninterrupted through the lens fibres.
Some degree of lens opacity is present in all older dogs (older than seven years of age); however, this is not always cataract. Nuclear sclerosis is an age-related progressive lens cloudiness that is commonly mistaken for cataract.
The age-related cloudiness is caused by a gradual increase in nuclear density as the lens does not stop producing more lens fibres; the lens itself does not increase in size, therefore the lens fibres become more densely packed (especially in the nucleus of the lens) with ageing.
Nuclear sclerosis is unlikely to significantly impair vision because although visual acuity may be reduced, the accommodative ability of dogs is much less than humans, so the impact on vision is much less and usually not recognisable clinically.
Nuclear sclerosis can be easily differentiated from cataract using distant direct ophthalmoscopy. Holding the direct ophthalmoscope set to your neutral setting (0 for most people without an ophthalmic prescription) to your dominant eye, examine the patient from an arm’s length and identify the tapetal reflection (Figure 1).

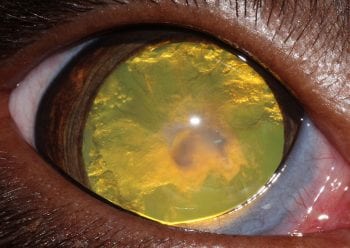
In patients with nuclear sclerosis, you will be able to see a clear tapetal reflection with no opacities; the lens nucleus may appear defined (Figure 2).
The tapetal reflection is maintained because the lens fibres, although more densely packed, maintain their highly organised structure, letting light pass through. In patients with cataracts, the tapetal reflection will be obscured either partially or fully by a black opacity (cataract; Figure 3).
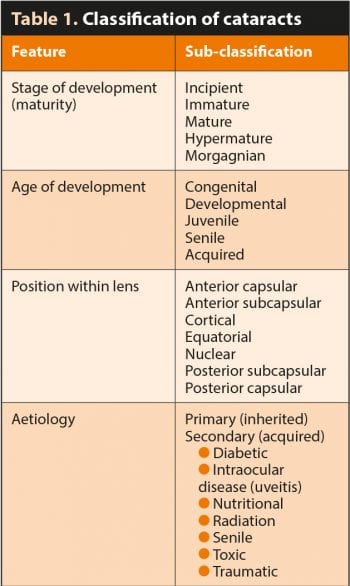
Cataracts can be classified based on stage of development (maturity), position within the lens, age of development and aetiology (Table 1). Classification based on maturity is most widely used; it is useful for monitoring and relevant to estimate the extent of visual impairment, as well as prognosis for successful cataract surgery.
The stages of cataract development are:
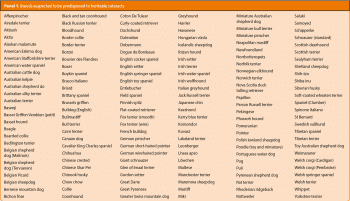
Hereditary cataracts have been demonstrated in many breeds (Panel 1). Hereditary cataracts are not always congenital, and the age of onset varies depending on the breed and causative mutation.
Congenital cataracts develop in utero and are present at birth. They may be inherited or secondary to an ocular developmental abnormality, such as persistent pupillary membrane, persistent hyaloid artery, microphthalmia or multiple ocular anomalies (a syndrome characterised by multiple ocular anomalies).
With the exception of those associated with persistent embryonic vasculature, congenital cataracts are usually seen in the nucleus of the lens (as this part of the lens forms while in utero).
Senile cataracts are common in dogs. The age of onset varies with breed; Williams et al1 reported that all dogs older than 13.5 years of age will have some degree of cataract on close examination.
Cataract development is a common complication of diabetes in dogs; it has been reported that 80% of dogs with diabetes will develop cataracts within 16 months of diagnosis; 60% of these develop within 6 months of diagnosis2.
In hyperglycaemia, excess glucose reaches the lens. This glucose overwhelms the normal metabolic pathway and is shunted to the aldose reductase pathway, and the end product is sorbitol.
Sorbitol is a relatively large molecule and is unable to cross the lens capsule, so accumulates in the lens. Sorbitol accumulation draws water into the lens from the aqueous humour via an osmotic gradient, causing hydration of the lens fibres and cataract formation3.
The cataract is often described as tumescent due to this water ingress, and can be sufficient to rupture the capsule in some animals. This is usually accompanied by an aggressive uveitis due to leakage of large amounts of antigenic lens proteins – this is referred to as phacoclastic uveitis.
A relationship between diabetic control and cataract formation has not been found; therefore, even with perceived good control of diabetes, cataracts still occur4.
Trauma that penetrates the lens capsule – such as cat claw or thorn injury – allows water to enter the lens and hydrate the lens fibres, causing a cataract. This is often accompanied by an aggressive uveitis due to phacoclastic uveitis.
Exposure to radiation during radiotherapy (for example, as treatment for nasal tumours) affects dividing cells in the lens equator and causes cataracts6,7.
Cataracts can be caused by progressive retinal atrophy: it is thought the degenerating retina releases toxic compounds into the vitreous that cause cataracts; often this is in the posterior lens cortex, closest to the vitreous. Cataracts can also be seen secondary to chronic uveitis due to lack of nutrients or exposure to toxic metabolites and end products available to the lens from the aqueous humour5.
Nutritional cataracts are rare in companion animals and are caused by deficiency of essential amino acids in young animals fed inappropriate milk replacement formulas5.
The gold standard treatment of choice for canine cataracts that are significantly impairing vision is surgical removal. The success rate is higher for surgical removal of immature or mature cataracts compared to hypermature cataracts, so early referral is ideal8. If the cataract is not significantly impairing vision, close monitoring for progression of the cataract and signs of uveitis is recommended.
In dogs with congenital cataracts, early surgical intervention should be considered – particularly in cases where the cataracts are dense and/or extensive. Evidence exists that lack of visual stimulation causes irreversible abnormalities to the central visual pathway and visual cortex – and, therefore, amblyopia “lazy eye” can develop.
If the patient is not showing signs of visual impairment, monitoring of progression is warranted. Young patients undergoing cataract surgery will develop postoperative posterior capsular opacification; regrowth of cataractous lens cells on the posterior lens capsule that can become dense enough to impair vision, as lens epithelial cells are more virile in the young patient.
This lens epithelial cell regrowth is also able to induce a uveitic response. For this reason, a posterior capsulotomy (making a planned hole in the centre of the posterior capsule to avoid lens cell regrowth in the visual axis) is usually performed.
All cataracts have the propensity to invoke a lens-induced (phacolytic) uveitis; inflammation inside the eye due to leakage of lens proteins out of the lens capsule into the eye. Therefore, all patients with cataracts should be treated with topical NSAIDs (assuming no contraindications exist, such as corneal disease) twice‑daily long‑term.
Lens rupture can occur spontaneously in mature cataracts, as well as secondary to traumatic lens injury. Lens rupture is seen particularly in diabetic cataracts that are rapidly progressing and tumescent in nature.
Lens rupture results in acute and often severe phacoclastic uveitis. Ideally, diabetic patients should be presented for cataract surgery as early as possible after cataracts are detected, due to the rapid progression and high risk of lens rupture.
If lens rupture is seen, the patient should be referred as an emergency for lens removal to avoid painful and permanently blinding sequelae, such as secondary glaucoma and retinal detachment.
Prior to cataract surgery, it is imperative to determine whether the retina is functional. Surgery is not recommended if the eye will not regain vision.
The retina cannot usually be visualised well through the cataract; therefore, additional diagnostic tests should be carried out prior to surgery – electroretinography to assess retinal function and ocular ultrasound to rule out retinal detachment (as well as other abnormalities of the posterior segment that could influence success – for example, persistent fetal vasculature, extensive vitreal degeneration).
It is also important to control any lens‑induced uveitis prior to surgery to decrease postoperative complications.

The procedure is carried out under general anaesthesia using an operating microscope with equipment that is usually only available in a referral setting. The surgery involves entering the eye through a small incision in the peripheral cornea and making a controlled hole in the anterior lens capsule (capsulorrhexis).
The lens material is removed from the lens capsule by phacoemulsification (Figure 9). The lens capsule is left in place and an artificial intraocular lens (IOL) is placed in the capsular bag (Figure 10). The IOL replaces refractive properties of the lens and helps with focused vision.
Placement of an IOL is not always possible, such as in cases when the posterior lens capsule is torn or when significant lens instability exists. If placement of an IOL is not possible, the dog will still be visual postoperatively; however, focusing ability will be reduced and the dog will be far-sighted.
Intraoperative complications are uncommon, but include ocular haemorrhage; posterior lens capsule rupture, which can be associated with dislocation of lens material into the posterior segment; retinal detachment; damage to the corneal endothelium; and corneal ulceration.
Postoperative complications include uveitis and glaucoma; close monitoring of intraocular pressure and intraocular inflammation is important. Patients are usually hospitalised for 24 to 48 hours postoperatively. Postoperative care includes frequent topical eye drops and regular re-examination; therefore, this should be considered when assessing patient suitability for cataract surgery.
Generally, all dogs receive topical and systemic anti-inflammatory medication, which is gradually tapered over several months postoperatively. Because of the risk of potentially painful and blinding complications, lifelong monitoring post-cataract removal surgery is recommended.
At the University of Bristol, we are carrying out clinical research into the characteristics of intraocular inflammation in cataract patients. We hope to be able to use this research to develop more targeted biological therapies for uveitis in the future, as has been done in human medicine. Please contact us if you would like to learn more about the research we are conducting, or if you have any patients that may be candidates for cataract surgery that might be enrolled into the study.