16 Apr 2024
Chris Dixon talks through diagnosis and surgical options that can treat rhegmatogenous detached retinas in dogs, and even bring sight back.

Figure 4. Ocular ultrasonography is performed.
Retinal detachment can be a sudden, devastating disease with an acute loss of vision. Many possible causes of retinal detachment exist, and in the absence of verbal communication with our patients, the diagnosis is often not ascertained until both eyes are affected. Contrary to popular belief, many of these torn (rhegmatogenous) detached retinas can be reattached surgically and vision restored.
Making the diagnosis of retinal detachment can be difficult if the tissue cannot be directly visualised with an ophthalmoscope. This can occur in cases with corneal disease, cataract development or if the detachment is peripheral and outside the central optical axis. A pupillary light reflex (PLR) may be present with a total detachment, even if a negative menace response is noted. A positive direct or consensual PLR does not infer that there is vision, as the reflex does not require processing by the visual cortex. Application of a short-acting mydriatic, like tropicamide, is required to allow for complete fundic examination, and ocular ultrasonography is an invaluable tool in the detection of sub-retinal fluid accumulation.
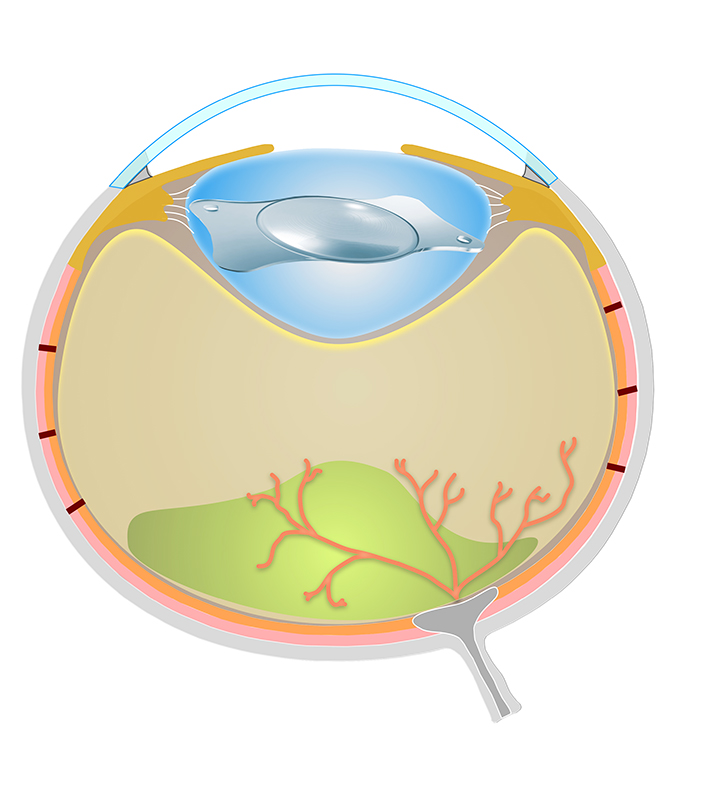
The clinical signs will vary depending on the cause of the detachment and the extent of the pathology. In cases of partial retinal detachment, the eye may appear outwardly normal, but with total retinal detachment, the neurosensory retina is unable to function and the patient will be blind in the affected eye. In more severe cases, the pupil may appear dilated, a floating sheet may be seen inside the eye, and the patient may collide with obstacles on the affected side (Figures 1 and 2).
Ocular ultrasonography can be performed either through the eyelids, or by gentle direct contact on the cornea following the application of topical local anaesthetic – for example, proxymetacaine – and a liberal quantity of a suitable ultrasonographic coupling gel. The depth of the image should be set to approximately 5cm, and the focus point aligned with the posterior pole of the eye or vitreal body.
Veterinary ophthalmologists will use high frequency (more than 16MHz) ocular ultrasound probes, but a reasonable image can be obtained with most probes and most machines scanning at 8MHz to 12MHz.
The aqueous humour and the vitreal body should appear anechoic, and a retinal detachment may be detected as a hyperechoic line. It is important to scan in multiple planes, as a dorsally detached retina will be folded over the optic nerve head and can be easily missed. The author would recommend dividing the ocular surface into a clock face and systematically scanning through the central and peripheral axes. The classic “seagull” appearance (Figure 3) can occur if the neurosensory retina (NSR)remains attached around the optic nerve head and ora ciliaris, but large tears can result in folding and twisting of the retina with multiple irregular hyperechoic lines.
The NSR is inserted at the ora ciliaris retinae and around the optic nerve head, but otherwise it relies upon hydrostatic pressure, and support from the vitreal body, to remain in contact with the underlying retinal pigment epithelium (RPE).
Throughout life, a potential space remains between the NSR and the RPE, and fluid accumulation within this space can lead to a retinal detachment.
Retinal detachments can be classified as either partial or complete, and either rhegmatogenous with a tear in the NSR, or non-rhegmatogenous. Rhegmatogenous detachments are either primary, which are spontaneous, or secondary, which are related to other ocular disease, including trauma, glaucoma, inflammation or surgery.
Non-rhegmatogenous detachments can be classified as exudative, with disruption to the blood ocular barrier, or form following the development of traction bands within the vitreous.
Some breeds are prone to hereditary retinal diseases that may allow a retinal detachment to occur. Retinal dysplasia (RD), collie eye anomaly (CEA) and persistent hyperplastic primary vitreous (PHPV) are all congenial diseases that may develop subsequent retinal detachments.
The author’s clinic has found that the shih-tzu, Lhasa apso and Italian greyhound are over-represented with spontaneous rhegmatogenous retinal detachments. The vitreous is approximately 99% water, contains a network of insoluble protein fibrils and occupies nearly 80% of the volume of the eye. The normal canine vitreous is a “nuclear type” and has an increased density centrally.
If liquefaction of the peripheral vitreous occurs, the collagen fibrillar insertions into the internal limiting membrane can be disrupted, leading to retinal detachment. Machemer et al noted that liquid vitreous moves counter to the direction of the eye, and it has been postulated by Vainisi and Wolfer that the risk of detachment increases in dogs that shake their heads vigorously.
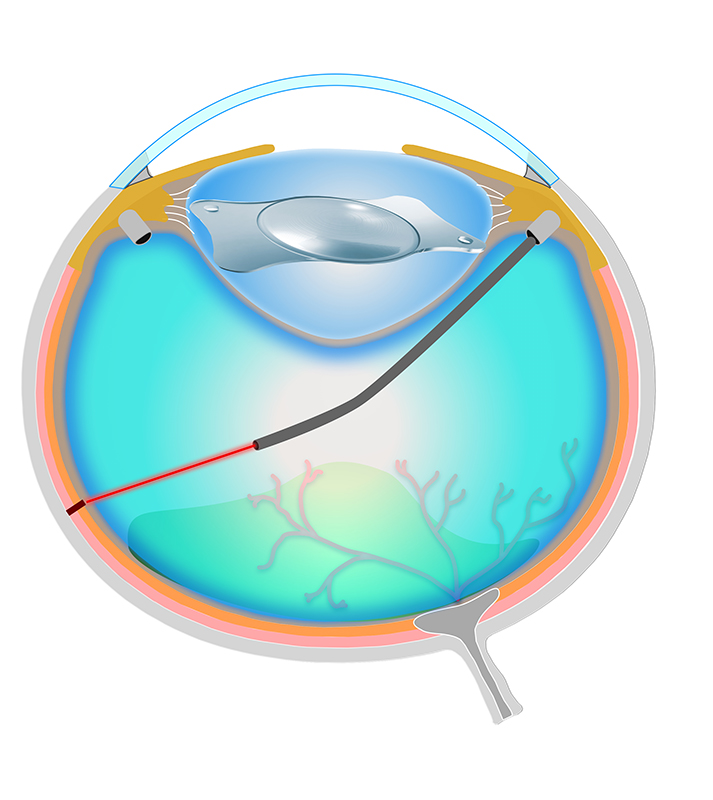
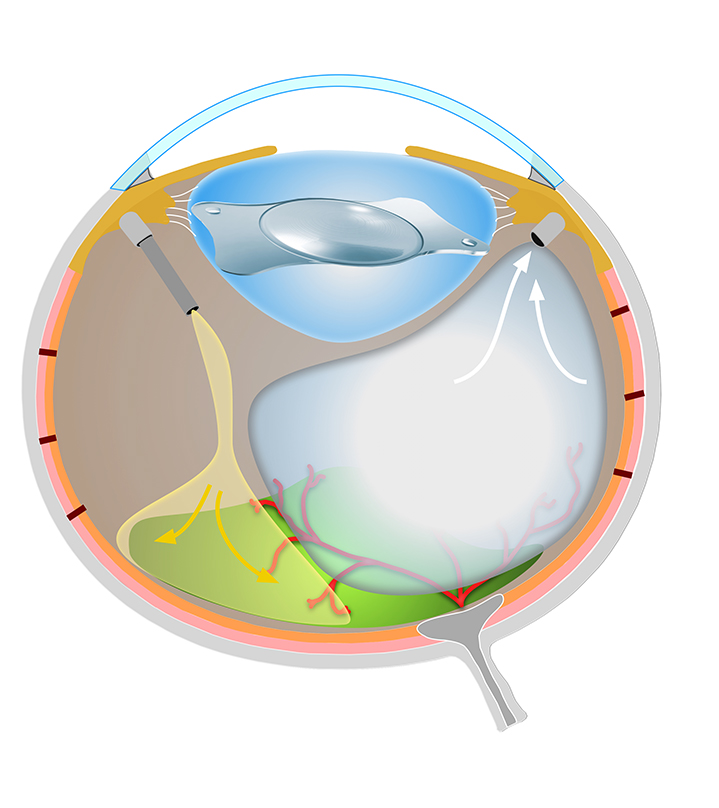
To perform retinal reattachment surgery, a complete posterior vitrectomy must be achieved. This is a complex procedure that normally begins with removal of the crystalline lens by phacoemulsification, and insertion of a prosthetic intraocular lens (identical to cataract extraction). Following closure of the corneal incisions, the eye may be partially proptosed to allow for adequate exposure of the scleral tissue; this may prove difficult in non-brachycephalic breeds.
Three self-sealing ports are inserted through the pars plana, carefully avoiding the vascular intrascleral plexus known as the circle of Hovius. These ports allow for the insertion of instrumentation and a light source into the posterior segment. Visualisation of the vitreal body and NSR is achieved with additional optical systems attached to the operating microscope, effectively allowing for inverted indirect ophthalmoscopy.
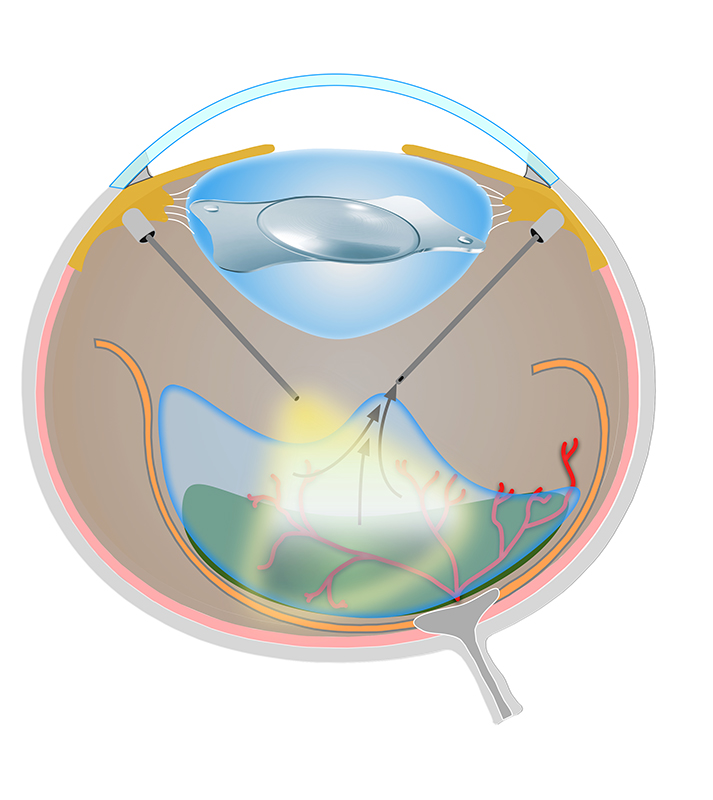
The first part of vitreoretinal (VR) surgery is the complete removal of the vitreal body, haemorrhage and inflammatory debris from the posterior segment. This process involves the use of a 23G pneumatically driven high-speed vitrectomy handpiece, which can remove the tissue at more than 5,000 cuts per minute.
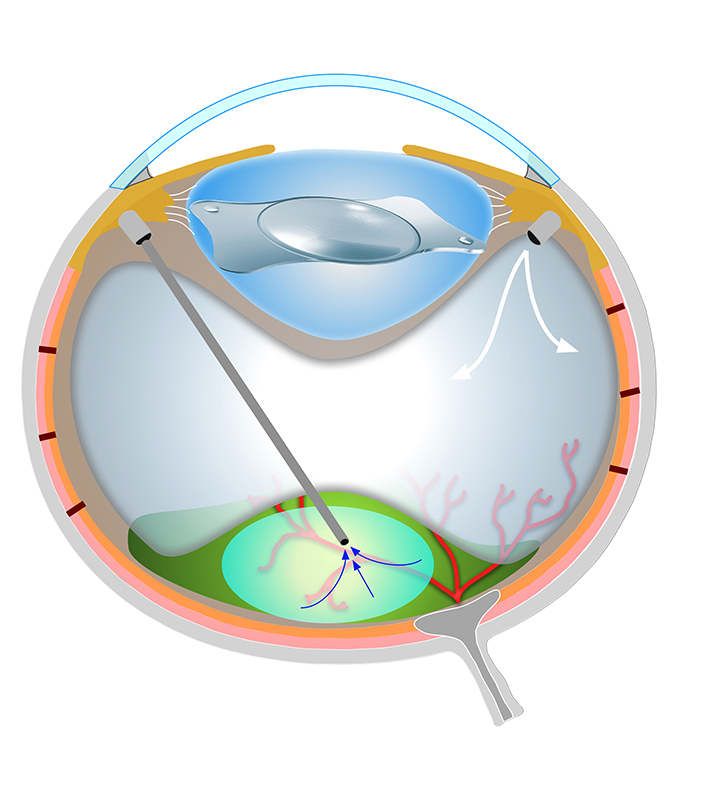
The VR machine maintains the intraocular pressure and the vitreous is replaced with a balanced salt solution. The free-floating NSR is flattened against the RPE with the injection of a heavy perfluorooctane liquid, and a laser retinopexy is performed to seal around any tears in the tissue.
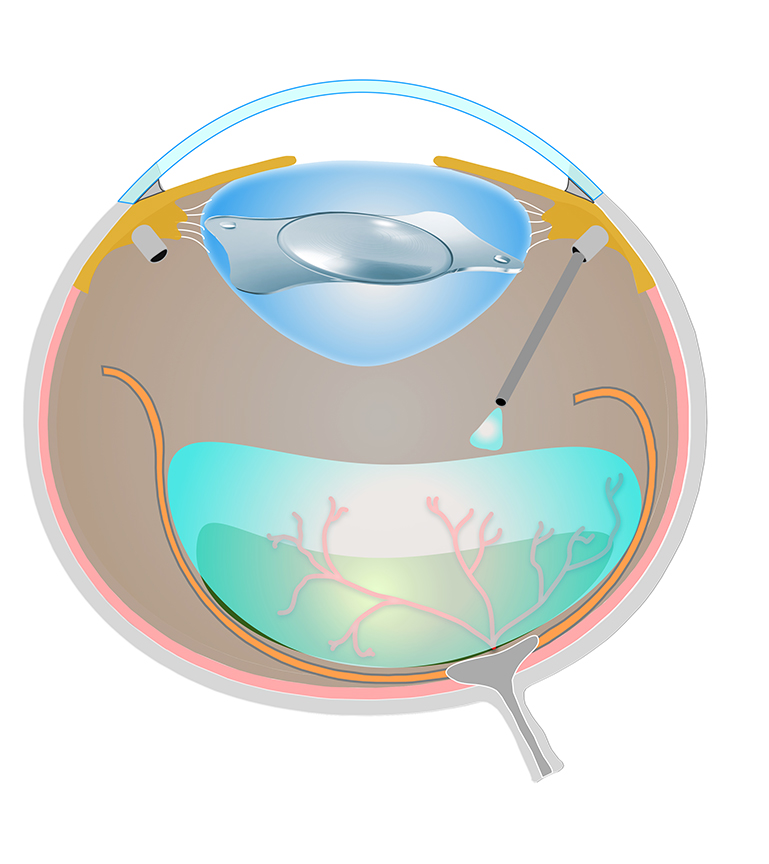
The heavy liquid is toxic to the NSR and cannot be left in situ, and it is removed with the delivery of medical air into the posterior segment. Human patients are commonly left with a gas bubble that will gradually be resorbed over several weeks, and are instructed to keep their head in a particular position during this period. However, if the gas bubble moves out of position, the retina may re-detach, and our canine patients would be not compliant for this option.
As an alternative to the dissolving gas bubble, the posterior segment is filled with a high viscosity silicone oil (SiO). The SiO has a specific gravity of 0.971, which is less than water, allowing for a permanent floating bubble that supports the reattached NSR (Figures 6-11).
Historically, canine retinal reattachment surgery has had limited success, but this has changed due to the rapid advancement of technology within the past 10 years. The new range of dedicated VR machines allow for smaller port placement (23G-27G), the delivery of fluids, gas and oil without a significant change in intraocular pressure, and a high-speed vitrectomy cut rate.
Unfortunately, these sophisticated machines can cost more than a new CT scanner, have extremely high consumable costs and require specific surgical training.
The canine retina will gradually degenerate in a detached state, and it is prudent to recommend early intervention to increase the chance of replacing viable tissue. The rate of degeneration is thought to be multifactorial, and is most likely to be dependent on maintaining adequate vascular perfusion. The author’s team has found that in the absence of a menace response, a direct pupillary light reflex is a positive prognostic indicator.
Published studies have reported success rates of 72% to 92%, but very few experienced veterinary VR surgeons exist globally. Not all cases are suitable for surgical intervention, and careful ophthalmological assessment is required prior to embarking on an operation.
If you have a case with a retinal detachment or would like further advice regarding this disease, the author’s team can be contacted at [email protected] or visit tinyurl.com/bdfv8xsv for a video showing surgery.