10 Mar 2020
Maria-Christine Fischer DVM, DipECVO, MRCVS in the final of a two-part article, discusses essential steps for examining and treating this ocular condition.

As described in part one of this article (VT49.49), cataracts are the leading cause of vision loss in dogs.
Due to great progress in cataract surgery in the past few decades, lens opacities can now be removed surgically, with reported success rates of up to 90% one year postoperatively1-3. This article describes essential steps for examination and treatment.
Cataract surgery is an elective procedure performed under general anaesthesia. Proper selection of patients is essential for successful surgical outcome. A thorough history, physical and ophthalmic examination helps to determine if the patient is a suitable candidate for cataract surgery.
Age, breed, and a history of systemic and ocular diseases – including all recent and current medication – can help determine possible underlying causes for cataract development (for example, diabetes mellitus) and potential risk factors for the general anaesthetic.
The affected patient should display significant visual deficits to justify cataract surgery. As dogs can adapt very well to slowly progressive loss of vision, the degree of visual impairment may be difficult to determine for the owner.
Dogs with visual deficits may present with a change of character (more insecure, cautious, aggressive, less active or a tendency to stay closer to the owner), bumping into stationary objects in familiar or new environments, finding it difficult to catch toys or treats, or showing differences of behaviour in dim and bright light conditions.
The onset and progression of visual deficits can provide further information on the stage of the cataract, its progression and potentially its aetiology. In cases of progressive retinal atrophy, for example, the patient typically presents with night blindness (nyctalopia)4 with or before a lens opacity is noticed by the owner.
When presented for cataract assessment, a thorough physical examination is helpful to determine systemic diseases that could cause a cataract (for example, diabetes mellitus) or interfere with a general anaesthetic and the postoperative management (for example, cardiac disease, renal insufficiency, hepatopathy, coagulopathies, systemic hypertension, hyperadrenocorticism and diabetes mellitus).
Inflammatory processes such as blepharitis, dental disease, otitis and cystitis may increase the postoperative risk of infection and may require pre-operative treatment5,6. Patients with neoplastic disease may also not be suitable for cataract surgery.

When performing an ocular examination, a systematic approach is essential.
The examiner should start observing the patient when navigating in the consult room. An obstacle course in dim and bright light conditions can also provide clues as to the degree of visual impairment. Vision testing should also include menace responses and subsequent visual tracking test, maze testing and visual placing responses. Direct and indirect pupillary light reflexes performed in a darkened room can help evaluate retinal function and abnormalities of the iris. Miosis may be present due to uveitis; dyscoria due to synechia; and mydriasis due to increased intraocular pressure, iris atrophy or loss of retinal function.
Subsequently, it is recommended to evaluate the quantity and quality of the tear film via the Schirmer tear test and tear film breakup time. Schirmer tear test values of more than 15mm/min and tear film breakup of more than 15 seconds are considered normal in canine patients7. Diabetic patients appear to be predisposed for keratoconjunctivitis sicca, and this can be exacerbated by the general anaesthetic, increasing the risk for postoperative corneal ulceration8.
When examining the eye, a focal light source and magnification (ideally a slit lamp or alternatively a direct ophthalmoscope), is required. The eyelids should be evaluated for their position, presence of distichia, eyelid masses and inflammation (Figure 1) that could cause corneal irritation or increase the risk of infection.
Corneal opacities such as corneal oedema, fibrosis, pigmentation and vascularisation (Figure 1) may interfere with visualising intraocular structures during cataract surgery. Corneal oedema related to endothelial dystrophy or degeneration may worsen postoperatively due to damage of the endothelial cells intra-operatively related to irrigation and thermal effects of phacoemulsification or postoperatively related to uveitis or glaucoma9.

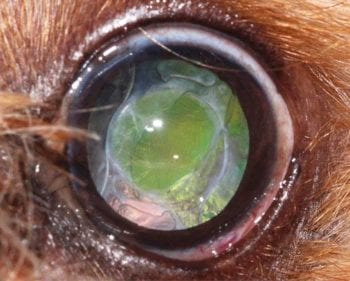
Lens-induced uveitis (LIU) presents as aqueous humour flare (Figure 2), miosis, congested episcleral vessels (Figure 3), endothelial precipitates, hyperpigmentation of the iris, posterior synechia (adhesions between iris and lens) and pigment migration on the anterior lens capsule.
Tonometry of the intraocular pressures should be performed prior to the application of mydriatic agents. Values of 10mmHg to 25mmHg are considered physiologic for dogs. Low or high normal to increased intraocular pressures can be suggestive for LIU or glaucoma, respectively. Blind patients due to chronic glaucoma are excluded from cataract surgery10. Combined cataract and glaucoma surgery can be performed in patients with increased intraocular pressure due to primary glaucoma, and for patients with an increased postoperative risk of glaucoma (for example, 30% rate of glaucoma after cataract surgery in terriers with lens luxation11. In this procedure (endocyclophotocoagulation), a diode laser is used to coagulate parts of the ciliary body endoscopically after phacoemulsification and implantation of an artificial intraocular lens. The partial destruction of the ciliary body results in decreased aqueous humour production12.
After increased intraocular pressure has been ruled out, the examination can proceed with dilation of the pupil via the short-acting mydriatic tropicamide.
Subsequently, the lens is evaluated for opacities and potential instability. Direct illumination, retroillumination and focal illumination with a slit can be helpful to assess the density, location and the stage of the progression (Figures 3 to 5). An aphakic crescent, lentodonesis and prolapse of the vitreous into the anterior chamber indicate instabilities of the lens. This lens instability can increase during phacoemulsification and may prevent implantation of an artificial intraocular lens in severe cases. Dog breeds predisposed for primary lens luxation are terriers, border collies, Australian cattle dogs and Shar Peis13-15. Patients with hypermature cataracts and LIU are at a higher risk for secondary lens luxation.

If possible, fundoscopy should be performed to rule out retinal degeneration and retinal detachments. Retinal degeneration is usually bilaterally symmetric and typically presents with attenuated retinal vasculature, hyperreflectivity of the tapetal fundus and a pale optic nerve head. Retinal degeneration has been reported as the most frequent cause for excluding patients from cataract surgery16. However, a more recent study17, and the author’s own experience, have shown good improvement of visual performance following cataract surgery in cases with early progressive retinal atrophy.
If the fundus cannot be examined thoroughly due to the lens opacity, retinal function should be evaluated with electroretinography (ERG; see further on).
We recommend performing ocular ultrasound, gonioscopy and electroretinography prior to cataract surgery.
Ocular ultrasound can usually be done in the gently restrained, conscious patient. A 10mHz linear transducer is used with sterile coupling gel in direct corneal contact technique, under topical anaesthetic (for example, proxymetacine eye drops). The axial length of the globe and the size of the lens are measured. In addition, the eye is evaluated for vitreal degeneration, retinal detachment, spontaneous lens capsule rupture and persisting embryonal blood vessels. Vitreal degeneration may predispose certain dog breeds such as shih-tzu, Boston terrier and poodle for retinal detachment18-19. In case of a recent retinal detachment, ocular light reflexes and the retinal function on electroretinography may still be positive20. Patients with complete retinal detachment are in general excluded from cataract surgery.
Therefore, it is important to perform ocular ultrasound if fundoscopy is no longer possible due to the lens opacity. A lens capsule rupture results in an increased intraoperative risk dislocating lens fragments into the vitreus, which can lead to persistent uveitis, retinal tears and retinal detachment9. In addition, it might not be possible to implant an artificial intraocular lens, in which case the patient would be farsighted.

ERG evaluates the retinal function and records the electrical response of the retina to light stimuli. A non-recordable or reduced retinal response may be caused by progressive retinal atrophy or retinal detachment. A reduced retinal function can also be concurrent with diabetes mellitus in 43% of the cases21 or with lens induced uveitis22, in which cases it can improve postoperatively.
Gonioscopy is used to evaluate the iridocorneal angle. Although no direct correlation between a narrow iridocorneal angle and postoperative hypertension or long-term glaucoma has been reported, it may influence the surgeon’s approach or prognosis9.
As oxidation plays a role in cataractogenesis, it has been suggested antioxidants may help prevent, delay or reverse cataracts. However, clinical evidence for the efficacy of these drugs is poor. It is important owners are not misled into thinking cataract surgery can be avoided or delayed. Kinostat may be an exception to other “anticataract drugs”.
This aldose reductase inhibitor is applied topically three times a day and has been shown to be effective for inhibiting diabetic cataracts in dogs23-24. This drug is awaiting Food and Drug Administration approval.
At the time of writing, extracapsular lens, extraction remains the treatment of choice and phacoemulsification, followed by implantation of an artificial intraocular lens is the gold standard method5. The procedure is performed under general anaesthetic with the aid of an operating microscope. After a 2.8mm to 3.2mm perilimbal corneal incision, a circular rhexis of the anterior lens capsule is performed. The phacoemulsification tip is then inserted into the lens capsule bag, and used to emulsify and aspirate the lens nucleus and parts of the cortex. The remaining cortex is then removed via automated irrigation and aspiration. Subsequently, a foldable artificial intraocular lens (IOL) with a power of 41 diopters is implanted into the lens capsule bag to achieve postoperative emmetropia (focused vision). Dogs that remain aphakic (in which an IOL has not been implanted) have a severe hyperopia (farsightedness) of approximately 14 diopters25. Dogs that are left aphakic, however, seem to adjust well and regain fair to good vision postoperatively due to removal of the opaque lens.
Cataract surgery is recommended as soon as visual deficits associated with the lens opacity become obvious5. This occurs commonly in the immature stage of progression. Patients with rapidly progressive cataracts where loss of vision is imminent may also be considered surgical candidates9. Early cataract surgery is especially important in diabetic cataracts where rapid swelling of the lens fibres can lead to spontaneous lens capsule rupture21. Long-standing and hypermature cataracts with lens-induced uveitis, lens capsule plaques and instabilities of the lens zonules have a less favourable outcome due to potential intraoperative and postoperative complications26-29.
The clients’ and patients’ compliance play an essential role in the decision for cataract surgery. Postoperative treatment and regular re-examinations are time consuming, and associated with a significant financial investment, but have a great impact on the outcome of cataract surgery. Very lively, uncooperative or aggressive patients that are difficult to medicate and cannot be kept quiet in the immediate postoperative phase may not be suitable candidates.
In addition, the client has to be made aware of potential risks and complications associated with cataract surgery. The success rate is reported to be as high as 80% to 90% over the first year. Short-term complications include uveitis, transient postoperative, ocular hypertension, wound dehiscence, corneal ulceration and hyphaema. The most common long-term complication is posterior capsule opacification, which rarely results in clinically apparent impairment of visual acuity (Figure 6). Glaucoma or retinal detachment can, however, eventually lead to loss of vision, may require removal of the globe and are associated with further costs.
It also has to be taken into account that patients with unilateral cataracts may not display obvious visual deficits and cataracts in young animals may undergo spontaneous resorbtion resulting in return of hyperopic vision30.
In cases where cataract surgery is declined, the client should be advised about potential complications associated with the cataract (see part one). Long-term monitoring and treatment are recommended in these cases. A study27 that compared success rates of different treatment options including no treatment, topical medication and cataract surgery over 2.3 years found that cataract surgery (independent of the stage of cataract progression) had the highest success rate. Topical anti-inflammatory treatment had four times higher failure rate (defined as discomfort, glaucoma, lens luxation, enucleation or euthanasia) when compared to surgery. The failure rate of untreated eyes was 65 and 255 times higher compared to medically and surgically treated eyes, respectively.
Cataracts are the most common cause of visual deficits and blindness in dogs. Cataract surgery has great potential to improve quality of life for the patient. The success rate of extracapsular lens extraction via phacoemulsification has a success rate of 80% to 90% over the first year postoperatively and a thorough examination, early surgery and diligent postoperative care have a great impact on the outcome. However, not every patient is suitable for surgery and phacoemulsification remains an elective procedure.
Most dogs adjust to loss of vision well, but need long-term monitoring and medical treatment. Left untreated, lens induced uveitis, glaucoma, phthisis of the globe, retinal detachment and lens luxation are possible complications of cataracts, which may lead to pain and/or irreversible loss of vision.