30 Aug 2022
Robert Weekes BVSc, MRCVS and Gerald Olivares DVM, MVetMed, DipACVIM, MRCVS discuss the case of a four-year-old male neutered border collie in this Case Notes piece from Vet Times.

A four-year-old male neutered border collie named Bo was presented to his first opinion practice with a week’s history of lethargy, exercise intolerance, weight loss, intermittent vomiting, and polyuria and polydipsia (PU/PD).
Investigations included blood work – namely complete blood count (CBC), serum biochemistry, coagulation times, vitamin B12, folate, trypsin-like immunoreactivity and canine pancreas‑specific lipase – and abdominal ultrasound.
These investigations revealed a stress leukogram, mildly increased basal bile acids, increased alanine transferase (ALT; 390U/L, reference interval 0U/L to 100U/L), apparent microhepatica and absent gall bladder.
Bo (pictured above) received amoxicillin/clavulanic acid and ursodeoxycholic acid, and was referred to the internal medicine service at Eastcott Veterinary Hospital. The only relevant previous medical history was an umbilical hernia repair at six months of age.
Bo was very bright and alert on physical examination. A 10% weight loss had occurred and the body condition score was decreased (BCS 3/9). The xiphoid process was absent on palpation.
The more relevant and specific problems in this case were the increase in ALT, absent xiphoid process and previous umbilical hernia (Table 1).
A CBC was performed at the referral consult and indicated a mild lymphopenia; it was otherwise unremarkable. Serum biochemistry revealed increased, but stable, ALT levels.
Bo’s gastrointestinal signs and concurrent PU/PD meant hypoadrenocorticism was possible. An adrenocorticotropic hormone stimulation test was performed, and this ruled out hypoadrenocorticism.
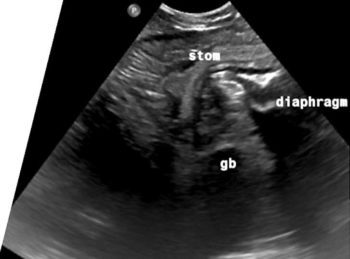
An abdominal ultrasound showed a ventral midline diaphragmatic defect with herniation of the stomach, proximal duodenum, spleen, pancreas and a portion of the liver, including the left lobes and the gall bladder (Figure 1).
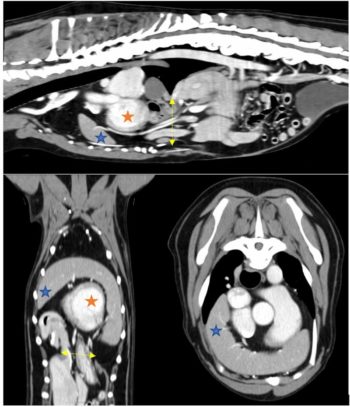
Due to the findings on the abdominal ultrasound, it was decided to perform a CT scan to further characterise the diaphragmatic defect and precisely locate all displaced viscera. This revealed a large 4cm defect in the diaphragmatic midline slightly caudal to the foreshortened and abnormally shaped sternum (Figure 2). The spleen, gall bladder, pancreas, pyloric antrum and proximal duodenum were all herniated through this defect, and likely sitting within the pericardial sac surrounding the heart ventrally – confirming a diagnosis of congenital peritoneopericardial diaphragmatic hernia (cPPDH).
Although not featured highly on the differential list, cPPDH is a recognised congenital defect that often involves herniation of organs into the pericardial space. Due to its nature as a congenital condition, it is often diagnosed early in a patient’s life, but, as occurred in this case, some dogs can live with a cPPDH for several years with no obvious clinical abnormalities.
In this patient, the authors believe the presenting signs (lethargy, exercise intolerance, weight loss, intermittent vomiting and PU/PD) were due to the visceral pain or nausea caused by herniation of abdominal visceral through the diaphragmatic defect.
An increase in ALT is a common laboratory finding in both cats and dogs with cPPDH, supposedly caused by trauma to the liver – as previously described in the literature1. The combination of diaphragmatic, pericardiac, body wall and sternal defects makes this a likely case of incomplete pentalogy of Cantrell2,3.
Both conservative and surgical options can be considered in the treatment of cPPDH cases.
A 2013 publication looked at the outcomes for dogs and cats with PPDH that received both treatment options4. No significant difference was found in long‑term survival time, but a larger proportion of cases with clinical signs attributable to the defect – as existed in this case – went on to be surgically managed.
This publication also showed the rate of surgical complications was low and the long‑term prognosis for resolution of clinical signs was good.
Since Bo had clinical signs that could be attributed to the cPPDH – and were progressive – surgery was recommended.
Bo underwent surgery for the diaphragmatic defect and herniated abdominal viscera.
A midline coeliotomy was performed and the peritoneopericardial hernia was confirmed, alongside herniation of the spleen, gall bladder and quadrate liver lobe. The quadrate liver lobe and gall bladder were easily reduced with gentle traction; however, the spleen was irreducible.
A caudal median sternotomy of the two most caudal sternebrae was performed to improve visualisation and access the herniated spleen. An omental adhesion between the spleen and cranial pericardium was identified, and was preventing reduction of the spleen. On further inspection, the omentum was found to be herniated through an additional defect in the midline of the cranial pericardium and was adhered to the cranial mediastinal structures (Figure 3).
A vessel sealing device was used to release the omental adhesion and the spleen was successfully reduced.
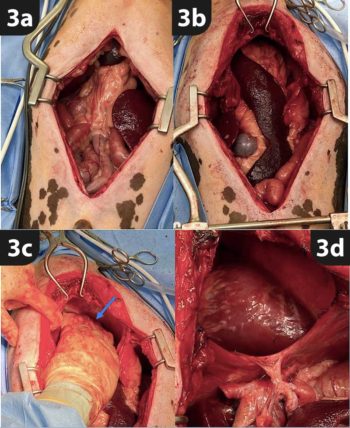
The caudal sternum was closed with 0 polydioxanone (PDS) figure of eight sutures. The diaphragmatic defect was closed with 2-0 PDS in a simple, continuous pattern, and air was drained from the pericardium via thoracocentesis.
The abdomen was closed routinely and the patient recovered in the intensive care unit.
Following an uneventful recovery, Bo was discharged three days post-surgery for strict rest at home for four weeks postoperatively.
At follow-up four months post-surgery, the patient was reported to be exercising at a level greater than before presentation and had a much better appetite. No other concerns existed.
cPPDH is a rare condition that can present with vague/non-specific clinical signs in young and adult dogs. Diagnosis is made through imaging of the abdominal and thoracic cavities by radiographs or ultrasound; however, CT scan can be helpful at achieving a definitive diagnosis and can be useful for surgical planning.
Although research has shown no significant difference in the outcome for patients that undergo surgery4, in some cases the improvement in clinical signs seen with surgical resolution of the hernia show it can be a viable option for the management of a cPPDH.
During the authors’ research, they found the combination of midline congenital defects can be grouped together into the pentalogy of Cantrell, a well-documented condition in human medicine, and is made up of five congenital defects affecting the sternum, midline abdominal wall, heart, diaphragm and pericardium. In this case, four of these defects were found – making this a case of incomplete pentalogy of Cantrell.
The lead author would like to thank the team at Eastcott Referrals for their involvement in this case, and especially the second author and Charlotte Howes for their input in this case report.
He would also like to thank Bo’s owners for consenting to sharing details of the case.