21 Jan 2020

Calcium deficiency problems are common in dairy cows and tend to increase in herds as milk yields rise. This is due to the sudden change in calcium demands for a milking cow when it begins lactation.
Slight hypocalcaemia occurs in most dairy cows during the adaptation process of lactation. However, this physiological process can go wrong at several stages and result in milk fever (parturient paresis). Clinical signs are a progression and, except most cases occur at calving, can be confused with other problems.
As the factors precipitating the clinical case are variable, a blood sample should be taken to confirm the diagnosis, and determine underlying causes and how to then prevent them in the transition period of other cows.
Treatment is usually successful, but many different strategies can assist in hypocalcaemia prevention. Following a case of milk fever, several other problems can potentially arise.
Probably more than three-quarters of all problems in dairy cows occur or originate around calving. This periparturient period is given various time lengths, but is often considered to be four to six weeks pre-calving and post-calving.
While physical problems are the main cause of dystocia, even then some parturition troubles are caused by metabolic disorders. However, soon after birth almost all problems are directly or indirectly related to the cow’s physiology and metabolism.
The major ones include diseases such as milk fever (parturient paresis), staggers or ketosis, or, more often, subclinical hypocalcaemia, hypomagnesaemia or hyperketonaemia.
In recent years, what has also become apparent is that they – and other deficiencies – are all, to some extent, linked. An attempt will be made to show some of these associations in the case of hypocalcaemia.
These metabolic conditions are not new, but in the past, when farms were small, they often occurred in one animal at a time on the farm and it was given appropriate treatment. However, little or nothing was done to investigate the causes or how to prevent them.
It is now recognised most of these conditions are herd problems and often considered to be “iceberg diseases”, being mainly caused by the management in the so-called dry period. Today, this term is seen by some to be pejorative, so it is now often described as the transitional or periparturient period.
These descriptions were to provide more gravitas, with the aim of impressing the farmer and elevating in importance this time period. It is, in fact, the most critical part of the cow’s production life cycle.
Traditionally, once an animal ceased lactation, it was more or less forgotten about. Many herds were autumn calving, so the dry cows were left out at grass until close to birth.
Their counterparts in the spring calving herds would be kept in yards and mainly fed on poor-quality roughage – often straw, with minerals and possibly a little cereal, molasses mix or cattle pellets to provide protein and some energy. A few days before calving, their ration was altered to include the lactation ration.
Some cows were “steamed up”, with the intention of not only familiarising the cow with the milking ration, but, hopefully, increasing early milk production from the stored fat reserves (Kelly, 2000).
As cow breeds started to change from Friesian to Holstein – with their milk yields increasing (often average lactation yields doubled in a few years) – and herds increased in size, the importance of metabolic disease and nutritional management became very apparent. Therefore, mistakes became a major herd issue and not a single cow problem.
An individual animal with a problem is, in fact, a herd problem, and it is important to determine the cause and rapidly introduce remedial measures. Therefore, for instance, 52% of UK dairy herds were in excessive negative energy in late pregnancy and 75.2% of UK dairy cows were affected in the first 20 days post-calving (Macrae et al, 2019).
Quite rightly, much is written about management in the transition period. All herds are different, so will have different nutritional, housing and management requirements – meaning any really useful plan needs to be tailor-made for the herd and not just taken off the shelf. The various objectives are often in conflict and, therefore, difficult to achieve on farm.
The ever-increasing size of most herds means animals have to be treated as groups. This is not ideal, as it would be much more advantageous to be able to treat each animal as an individual. Herds with lower yields are likely to have more “forgiving cows” in them than higher-producing ones (Atkinson, 2016).
All-in-all, the herd owner should be told it is worth spending some hours annually – prior to the start of the main calving season – to evaluate the success, or otherwise, of the preceding year’s transition management, and the differences in the current year imposed by the feeds available, production changes and management alterations.
In the 30 years to 2000, Kelly (2000) suggested that because of the increased milk yield in dairy cows, the incidence of milk fever rose from about 3% to more than 7%.
Records in the late 1980s onwards suggested the level of milk fever was about 8% (Esslemont and Kossaibati, 2000), although their recorded herds varied from 4.1 to 7.2 per 100 calvings.
A figure of approximately 2% to 5% milk fevers (range 0% to 10%, but up to 25%) has been found in Australian, European and North American studies (DeGaris and Lean, 2008), but almost 50% of cows in US dairy herds suffered from subclinical hypocalcaemia (Reinhardt et al, 2011).
Age is a risk factor for milk fever, rising by about 9% per lactation, with most cases occurring from the third lactation onwards. Cases can occur pre-calving (21%), within 48 hours post-calving (76%) and 3% after 48 hours.
An outbreak is considered to have occurred when 10% of cows need treatment, or, in low-incident herds, when cases have doubled. In both instances, investigation and remedial action need to be taken.
Most calcium (8.5kg; 99%) in the body is found in the skeleton. The rest is distributed in the various body tissues (0.01g), fluids (4.5g) and blood (3.6g; Goff, 1999; 2014).
Besides blood clotting, calcium is involved in a wide range of enzymatic activities, including nerve impulse transmission, muscular contractions and bone formation.
Several factors are involved in calcium absorption. The calcium content of the dry cow diet is about 70g/day, while that for the lactating cow is about 90g/day – resulting in the dietary supply increasing by a factor of 1.3 (Chamberlain and Wilkinson, 1996).
However, in the dry cow, diet absorption efficiency is about 33%, but rises to about 57% post-calving.
The requirements of the late pregnant 600kg cow are about 23g of calcium (14g maintenance plus 9g for the fetus); this is absorbed from the diet that probably contains about 70g calcium per day.
After calving, a cow initially producing 25 litres of milk post-calving will require about 44g calcium daily (14g maintenance, 30g for milk), or about double the pregnant cow.
The main problem is that available calcium reserves at calving only amount to about 12g (equivalent to about 10 litres of milk).
Losses to the cow occur primarily in the milk, and much less so in fetal growth, urine and other secretions being matched with that absorbed.
Pre-calving diets high in calcium reduce its rate of absorption and slow the post-calving adaptation process.
Under normal conditions, bone resorption plays a little role in regulating calcium levels until about one or two weeks post-calving. However, this alters if the cow receives a low-calcium diet in the run-up to calving, or when the cow experiences acidotic conditions in the pre-calving period.
The latter situation occurs in the negative dietary cation-anion difference (DCAD) diets.
Breeds of cow do appear to make some difference in hypocalcaemia, partly because of their milk yields and composition. This is why beef cows uncommonly show the problem, but it is prevalent in dairy cows. It is common in the Holstein, but probably mainly because of the high milk yield produced.
The Channel Island breeds are often considered to be more susceptible to milk fever, although the reasons why are unclear (Constable et al, 2016).
Oestrogen levels also restrict calcium mobilisation and these rise towards parturition, thereby reducing the adaptation process (Eddy, 2004). This is also why milk fever is occasionally seen later in lactation in cows around oestrus.
Diarrhoea can result in a reduction in mineral absorption, with negative results including a reduction in magnesium uptake. Likewise, magnesium deficiency can cause scouring.
Stress is often unquantifiable in its effects, but can lead to no or lower feed intake. Problems can arise when groups are altered, overcrowding is present, feed space per animal is insufficient, the diet is changed, or a constituent is altered, such as a forage batch.
It is bound to receptor sites in the rumen and intestine, and facilitates increased transfer of calcium across the gut by calcium-binding proteins. Bone resorption is also increased and more calcium is retained by the kidney.
When calcium levels become high, calcitonin is released from the thyroid gland, and can stop renal absorption of calcium and phosphorus, and stop osteoclast activity.
The problem arises because of the abrupt change from being in-calf to one where the cow is producing perhaps 25L or more of milk almost immediately. This results in a massive alteration in calcium requirements by the cow.
Unfortunately, in some cows their normally excellent calcium homeostatic mechanisms – involving absorption of calcium from the gut or by mobilising calcium from their skeleton – cannot keep up with the sudden drastic change. Although plenty of calcium is present in the body skeleton, it is not immediately available for use.
Calcium will also be available in the feed, but around calving, gut motility is reduced and often slow. Therefore, the change in calcium requirements requires the parathyroid gland (situated near the larynx) to start excreting parathyroid hormone (PTH) at increased levels, which, with available vitamin D, will start the process of increasing the calcium available for use in lactation by increased absorption of calcium from the digestive tract and bone.
Calcium resorption by osteoclastic activity can also occur in an acidic environment (Figure 1).
Vitamin D (cholecalciferol) is stored in the liver and relatively inactive. To assist in calcium and phosphorus absorption from bone, it has to undergo two hydroxylations to 1,25-dihydroxycholecalciferol. The first hydroxylation (to 25-hydroxycholecalciferol, or calcifediol) occurs in the liver and the second (1,25-dihydroxycholcalciferol) in the kidney. This dihydroxy form initiates active calcium transport across the duodenal brush border (Aitken, 2016).
This activation by 1,25-dihydroxycholecalciferol requires 16 to 24 hours; when it comes to bone resorption, it takes about 48 hours.
While it is obvious the main reason for milk fever is the sudden demand for calcium in the milk, it is not assisted by the normal physiological changes at calving:
In older cows, an increased delay in vitamin D activation can occur; fewer intestinal 1,25-dihydrocholecalciferol receptors are present to absorb calcium.
As the name implies, no signs exist in subclinical hypocalcaemia. Most cows adapt to normal calcium levels within about two days.
A study suggesting hypocalcaemia involved blood samples were taken within 48 hours of calving and it was considered to be present if calcium was lower than 2mmol/L (Reinhardt et al, 2011).
A short period of bodyweight loss occurs post-calving compared to cows with calcium levels in the normal range. Hypocalcaemia is seen more in the older milking cow and occurs in towards 50% of early lactation cows.
The significance of these incidence levels is unclear, but may suggest the transition period management needs to be reassessed.
As aforementioned, most clinical cases occur in the two days before and after calving, and usually this helps differentiate milk fever from other conditions.
However, it is still important to determine whether any associated problems are present, such as mastitis or whether the calving process (natural or assisted) has caused any physical damage to the cow.
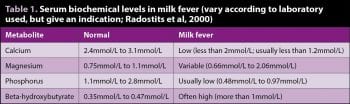
In all cases of milk fever, it is advisable to take a blood sample to confirm the diagnosis. It should – at minimum – be checked for calcium, magnesium, phosphorus and energy level (beta-hydroxybutyrate [BHB] or non-esterified fatty acids; Table 1).
Other tests may be thought necessary. Sometimes, response to treatment is used to confirm the diagnosis, but it is still worth checking the blood.
Often, milk fever is divided into three stages (Constable et al, 2016; Mann et al, 2019).
Usually, this stage is of short duration. Animals show appetite loss and variable excitability, with the hocks straight and often with a swaying lateral gait.
Muscle tremors occur around the head and limbs, and sometimes ear twitching and head bobbing occurs, which can make treatment difficult. Faeces are usually firm.
The heart rate, respiratory rate and rectal temperature are often within normal ranges.
This stage is difficult to treat effectively, as the cow’s signs often deteriorate post-treatment before the animal improves.
Differential diagnoses include:
This stage is variable in duration and can last a few hours to possibly two days. The animal is dull and less alert, in sternal recumbency – sometimes with an S-bend in the neck, or the head turned into its side.
Ruminal movements reduce, with a variable degree of bloat, constipation or faeces drier than normally expected on the diet, and anal sphincter relaxation. Pupils are dilated, but show a pupillary light reflex.
Usually, the heart rate is increased to more than 80bpm and of soft volume, respirations often end in a grunt, and rectal temperature may be low (lower than 38°C). However, lying outside or indoors in hot conditions may make the animal hyperthermic (Mann et al, 2019).
Differential diagnoses include:
The animal gradually loses consciousness and becomes comatose, goes into lateral recumbency, usually with marked bloat, and ruminal movements cease. The papillary reflex is usually absent.
Usually, the heart rate is increased to more than 100bpm and of soft volume, respirations are intermittent and rectal temperature is usually low (lower than 38°C).
Differential diagnoses include:
The overall duration of signs is very variable, but can be from about 10 hours to more than 24 hours. Therefore, if occurring at night, the cow may be found dead in the morning.
It should be remembered milk fever is a common cause of so-called sudden death.
Usually, between 8g and 12g of calcium are given by slow IV injection (Eddy 2004; Figure 2). A 400ml bottle of a 40% calcium borogluconate solution contains about 12g of calcium.
It is sometimes forgotten the solution should be warmed to about body temperature before giving, as, otherwise, problems can arise. The solution must also be given slowly or cardiac arrest can occur.
Today, some solutions also include calcium gluconate or calcium hydroxide. Some preparations also include magnesium salts, in the form of hypophosphite or chloride.
Blood calcium levels reach a peak at about 15 minutes after IV administration or after about 4 hours following SC injection (Braun et al, 2009; Blanc et al, 2014).
In cold conditions, absorption from under the skin can be slower, and placing the fluid in more than one site and massaging the injected area to disperse the fluid is helpful.
Following IV injection, the cow will often stand within half an hour and this assists in diagnosis. Relapses after successful treatment are quite common and may occur in between 20% and 30% of cases.
Obviously, the milk fever cow has to be treated, but the sudden introduction of a large quantity of calcium will interfere with the aforementioned physiological homeostatic mechanisms by inhibiting parathyroid hormone release and simulating calcitonin secretion, thereby reducing calcium resorption by the kidney and bone resorption (Goff, 1999). This can result in a relapse in signs.
It also occurs where a cow does not rise and is given repeated calcium injections, often by the farmer. In such cases, a blood test should be undertaken.
If the case clinically appears to have been corrected, any other complications should be rectified.
Otherwise leaving the cow to sort itself out may work, provided it is given access to fresh water and feed, or drenched with water or electrolyte solutions and possibly stimulants.
On occasions in these cases, the use of udder inflation has assisted, but requires being done ascetically to prevent infection entering the udder.
It is also recommended that following IV calcium injections, further calcium is provided orally (Mann et al, 2019).
Oral boluses can be used, but they caution against use of sodium propionate in the freshly calved cow as it may interfere with energy metabolism in an already hyperglycaemic cow and, therefore, result in appetite suppression.
Transition cow management is complex because one is trying to support the cow, but without blocking the normal physiological changes of parturition.
Several ways exist to assist the prevention of clinical hypocalcaemia; one or more of these are normally included in the transitional cow programmes. The methods used may need to change according to the feeds available and the body condition of the cows when drying off.
If a block calving pattern is in place, it is advisable that metabolic profiles are performed to examine the main metabolic parameters. It should involve groups of cows after two weeks of receiving the dry cow ration and at the end – especially when the diet is changed at that time, again allowing a period on the new feed before testing.
In year-round calving herds, the tests are often best performed following any major feed changes in spring and autumn. It is beyond this article to deal with this, but excellent practical papers by David Whitaker (2000; 2004) explain the procedures and their interpretations.
Various laboratories can undertake the tests, but one that also relates the findings back to the feeds provided is often the most helpful.

Body condition should be checked throughout lactation and especially about six weeks before the expected drying off date, so any remedial action can be taken in those too thin (less than 2.5) or too fat (more than 3.5; Figure 3). Ideally, they should be at a score of 3 at drying off.
Again during the dry period, animals should be regularly examined. The author’s experience is that a score of 3.5 can be too high on some rations. However, he has also found most farmers and their staff tend to overscore their animals.
It has been shown that acidifying the transition diet for three to five weeks prior to calving increases the calcium uptake from the intestines. They probably should not be used in heifers (Santos et al, 2019).
Various formulae are used in the DCAD calculations, but the usual one is:
Using all minerals as g/kg dry matter (DM), the DCAD (milliequivalents [meq]/kg DM)
(4.35 × sodium) + (2.56 × potassium) – (2.82 × chlorine) + (6.5 × sulphur)
The cations (potassium and sodium) make the cow alkalotic, but the anions (chlorine and sulphur) reduce alkalosis and may make the animal mildly acidotic.
At present, the recommended diet should produce -100mEq/kg DM to -150mEq/kg DM for three weeks before expected calving (Mann et al, 2019). If it is to be undertaken properly, an analysis of the dry cow ration for chlorine, potassium, sodium and sulphur is required. Then the subsequent pre-calving diet must contain sufficient calcium at about 1.5% DM.
Chamberlain and Wilkinson (1996) stated the DCAD diet can be achieved by the removal of all supplementary sources of potassium and sodium. If the balance is still more than +200mEq/kg DM, diet forages with lower potassium and sodium contents should be included.
When potassium levels are high, the cow may develop a metabolic alkalosis, which increases the potential for hypocalcaemia. When potassium content is about 1.4% then the chloride salts used to counteract it will reduce feed intake (Goff, 2014) – in such instances, a more palatable anion supplement is beneficial.
If necessary, ammonium chloride, ammonium sulphate or magnesium sulphate (Epsom salts) can be added. To avoid ammonia toxicity, the ammonium and magnesium salts should be mixed in a ratio of 1:1 with no more than 100g/day of Epsom salts. Higher levels may cause reduced feed intake and loose faeces can occur.
The use of DCAD diets does raise the blood calcium level on day of calving and afterwards, as well as lower BHB levels pre-calving (Lean et al, 2019).
Any method to reduce calcium intake during the dry period will result in an efficiency increase at calving. This can be, in part, achieved by feeding low calcium feeds (Table 2).
Most dry cow diets have a calcium:phosphorus ratio of about 2:1. The closer the dry cow feed can reach a ratio of 1:2 then the more intestinal calcium absorption will occur.
Increasing phosphorus and reducing calcium towards a ratio of 1:1 will increase calcium absorption. Phosphorus is relatively expensive, so supplementation is not used.
Looking at the aforementioned calcium physiology and in Figure 1, magnesium is needed at several key stages. It is used in the activation of vitamin D and the resorption of bone. It must be used carefully, as overuse will have a laxative effect and may result in competition with calcium for absorption.
Various calcium preparations exist – in the form of boluses, drenches and pastes – that can be given to the cow. Most involve one dose as the cow shows signs of – or at – calving, then a second dose 8 hours to 12 hours later or post-calving, depending on the product.
These products most commonly contain calcium carbonate, calcium chloride or calcium sulphate, with approximate calcium absorptions of 50%, 90% and 70% (Mann et al, 2019).
If used too early before calving then milk fever becomes a possibility because calcium absorption will be suppressed.
The content of calcium in milk is static, so reducing the volume milked from the cow will reduce calcium demand. However, if used, it is important to watch closely for mastitis.
Although frowned on by purists, an SC bottle of calcium with or without magnesium post-calving does appear to prevent milk fevers on some farms.
In most cases, it should not be repeated as it will be more likely to interfere with the calcium regulatory process.
IV calcium is little used as a preventive measure, but does disrupt calcium homeostasis compared to oral calcium supplementation (Wilms et al, 2019).
At one time, vitamin D and its derivatives were used by injection to assist in hypocalcaemia control. These are no longer used.
However, it is important that fat-soluble vitamins – such as vitamin A, vitamin D and vitamin E – are adequately supplied in the ration to ensure effective metabolism, supply in colostrum and improve the immune response.
It was suggested DCAD diets should be supplemented with vitamin D metabolites to reduce milk fever (Block, 1984). Recently, it has been shown supplementing the DCAD ration with 25-hydroxyvitamin D3 (3mg/day) activated neutrophils, reduced retained placentas, metritis and post-calving diseases (Martinez et al, 2018a), and increased milk yield (Martinez et al, 2018b).
It is suggested the early lactation ration should include 0.9% to 1% calcium, and 0.35% to 0.45% magnesium DM (Mann et al, 2019).
Although mainly aimed at preventing or reducing energy deficits, it would be expected any diet that encourages DM intake is less likely to result in hypocalcaemia cases.
We still have much to learn about when stress occurs in cows, but some points are obvious.
Although a herd animal, each change in group membership will alter the population dynamics, to a greater or lesser extent, for all members of the group – not just the lower ranking ones.
Good periparturient management addresses it as, by necessity, the group will be altering as cows calve and others join the group.
A practical approach has been described by Atkinson (2016).
Aspiration pneumonia can occur in the recumbent stages of milk fever, following regurgitation of ruminal contents and their inspiration into the lungs.
A temporary reduction in bodyweight will occur, but no long-term loss exists.
Animals that have had milk fever may be more likely to be culled because of the effects of the problem, but also as a result of the direct and indirect consequences.
The information available suggests a relationship exists in early lactation, but not late lactation.
Milk fever is a cause of apparent sudden death in dairy cows.
A relationship exists between left displacement of the abomasums and milk fever. However, factors causing displacement – such as fatty liver, hyperketonaemia and the diet – also affect milk fever levels.
Downer cow syndrome includes many different causes. Surveys have shown a variable proportion of those in early recumbency show low circulating calcium levels. This may be because they are slow responders to calcium homeostasis return, insufficient or overtreatment, and interaction with other metabolic or deficiency problems.
Hypocalcaemia can delay the calving process, causing uterine inertia and, therefore, causes subsequent calving difficulties in some cases.
Variable evidence exists about the effect of hypocalcaemia on fertility, but a recent paper (Mahen et al, 2018) has suggested ionised calcium concentration at calving was associated with increased chances of the cow being served and conceiving.
Some studies have shown a variably increased risk of ketosis following milk fever.
Hypocalcaemia is related, at times, to energy deficit and fatty liver – leading to alterations in mineral metabolism, such as hypomagnesaemia. This shows the importance of nutrition during the dry period.
Milk fever does lead to mastitis cases because of impairment of immune function.
The lack of muscular function allows a relaxation of the teat sphincters; therefore, pathogens can enter the udder in sternal and lateral recumbent cows.
Milk fever cows may also not be milked for a period while ill, or only partly milked out. The odds ratio for mastitis is about 8.1 and the risk of acute clinical mastitis is about 1.5.
A relationship appears to exist between metritis and milk fever. Various reasons may exist for this, including the relationship with energy deficiency and fatty liver. This may be due to impaired immune function.
Some cows appear to have suffered sudden death as they are found dead overnight. Other cases will occur during and after treatment because of various problems, including cardiac arrest.
A case fatality rate from downer cows due to milk fever is put at between 20% and 67% (Constable et al, 2016).
An increase in retained placentas occurs following milk fevers, but many other potential reasons exist for the problem.
Many cows that develop uterine prolapse have – or have had – hypocalcaemia.
Milk fever has been known about since the 18th century, but still causes problems today. It is exacerbated by the high yields now expected from dairy cows.
Hypocalcaemia is also related to other problems and has resulted in many control measures, all of which can assist. However, attention to detail and treating each cow as near an individual as possible are key factors in prevention and control.
Hopefully, this will prevent some or all of the cascade of negative events that can occur post-calving.