1 Oct 2018
Emily Haggett examines the clinical signs in presenting foals with this disease and its diagnosis treatment and prognosis.

Neonatal maladjustment syndrome (NMS) is one of the most common diseases affecting foals in the neonatal period.
The disease has been given many names over the years, such as dummy foals, perinatal asphyxia syndrome (PAS), barker foals and wanderer foals. This reflects the fact the exact underlying aetiology was unknown. Over the past few years some exciting discoveries have been made about the disease, which has helped to advance our understanding and treatment of affected foals. This article runs through the aetiology, clinical signs and treatment of the condition.

Historically, NMS has been attributed to hypoxic-ischaemic injury at around the time of foaling. Most commonly, this occurs during the foaling process, when problems such as fetal malpresentation, or premature placental separation cause delayed delivery and a reduction in blood supply to the foal. This is undoubtedly the underlying cause for some foals with the condition and is often easy to diagnose based on a history of a difficult delivery or prolonged dystocia (Figure 1).
However, the condition also occurs in foals that have had a seemingly normal delivery. In these foals it has been suggested abnormal compression of the umbilical cord, or some other factor not visible externally, exists.
In foals that have experienced a significant hypoxic episode, a complex cascade of events are initiated, including cellular energy failure, acidosis, glutamate release, intracellular calcium accumulation, generation of free radicals and, ultimately, cell death via necrosis or apoptosis. A second round of cellular injury occurs after the primary event as a result of calcium influx, excitatory neurotoxins, inflammatory mediators and oxygen-free radicals.
The organs most commonly affected by hypoxia include the brain, kidneys and intestinal tract. Foals that have experienced significant hypoxia tend to show severe clinical signs and have a poor prognosis for survival. Postmortem examination of these foals demonstrates evidence of hypoxic tissue injury and neuronal cell death. This mirrors the situation in human medicine where infants that have experienced significant birth hypoxia often have an increased mortality rate and are likely to suffer from long-term neurologic dysfunction.
Most foals with NMS make a rapid and complete recovery within two to five days of supportive care. This suggests the condition in these foals is caused by a different aetiology. In the author’s opinion, this condition may be better split into two syndromes – PAS for foals that have experienced a hypoxic event, and NMS for foals that have no history or suspicion of birth hypoxia.
Recent evidence suggests NMS occurs when foals fail to complete the normal birth transition process and don’t fully adapt to extrauterine life. In some foals, this transition process starts normally and then falters. In a normal foal, the hypothalamic-pituitary-adrenal (HPA) axis produces a large number of progestagen-based steroids that reach high concentrations shortly before foaling. It is proposed that high levels of these steroids at the time of foaling help suppress activity during parturition to prevent injury to the mare and foal. In a healthy foal, the final maturation of the HPA axis causes the activation of enzymes that convert these compounds to cortisol and its derivatives. This is responsible for the final maturation of many organ systems. Concentrations of progestagens then fall rapidly after foaling to near negligible levels by 48 hours of age.
In foals with NMS, something goes wrong with this process. Progestagen concentrations remain high after foaling or begin to fall and then rise again sharply. The exact trigger for the dysfunction in these pathways is not yet known, but it is likely many factors play a role. These factors may include systemic inflammation, hypoxia, abnormal delivery or placental abnormalities. In some foals that develop NMS, foaling has been observed to be unusually rapid, raising the possibility that the physical pressure of the birth canal may be an important stimulus for these normal maturational pathways. In foals that recover from NMS, progestagen concentrations drop in line with their recovery.
One of the important discoveries over the past few years is the role of high progestagen concentrations in the clinical signs of NMS. Many of the progestagen compounds are able to cross the blood-brain barrier and have neuroactive effects. These compounds, or the imbalance of these compounds, may directly cause some of the observed neurologic signs. Experimentally, infusion of certain progestagen compounds can cause sedation and reduced consciousness in healthy foals.

NMS affects foals between one to three days of age. The most common clinical signs are neurologic, but the syndrome can affect many body systems and, in severe cases, leads to multi-organ dysfunction. Foals with this condition exhibit a wide range and severity of clinical signs. Affected foals may be normal at birth and then go on to develop clinical signs in 12 to 48 hours. These tend to be less severely affected. Some show signs of the syndrome immediately after birth and, thus, tend to have more severe disease and a poorer prognosis.
Neurologic signs are often the most common (Figure 2 and videos at foot of article). These can range from a foal that appears slightly “slow” to a foal with marked obtundation or uncontrollable seizures. Common signs include loss of suck reflex and poor teat searching, persistent chewing movements, aimless wandering, altered mentation, abnormal head carriage, reduced interaction with the mare or the environment, hyperaesthesia, weakness or rapid exhaustion, inability to stand or stay standing. More severe signs include central blindness with anisocoria, opisthotonus or hypotonia, seizures and coma.
Other body systems are commonly affected. Respiratory signs can include periods of apnoea, abnormal breathing patterns, or barking vocalisation (rare), shallow tachypnoea and/or dyspnoea. Some of these signs relate to abnormal central control of breathing rather than primary respiratory disease. In foals that become recumbent or develop secondary sepsis, primary respiratory disease with atelectasis and ventilation/perfusion mismatch can occur.
Gastrointestinal signs are also common and range from mild colic to severe ileus. Some foals simply have reduced intestinal transit time and faecal output, and other foals become completely intolerant of enteral feeding.
Renal signs range from mild oliguria to complete anuria. Complete anuria can occur in foals following significant hypoxia. This is very difficult to manage and is often associated with high mortality. Endocrine and metabolic dysfunction is also common.
Diagnosis relies heavily on clinical signs and the exclusion (or inclusion) of other conditions. Careful physical examination and an accurate history usually give a good indication as to the likelihood of the disease. Haematologic and biochemical analysis, and measurement of blood pressure, blood gases and blood lactate levels, will help determine the degree of involvement of different organs and help determine the severity of the disease.
Progestagen concentrations can also be measured. Ultrasound can be useful to analyse the extent of gastrointestinal involvement. In foals suspected to have experienced true hypoxia, measurement of CSF pressure, or ultrasound to measure the diameter of the spinal cord have been suggested to determine whether intracranial pressure is increased. Advanced imaging, such as MRI or functional brain scans, may be useful in the future.
The majority of foals with NMS will survive if given early and appropriate supportive care (Figure 3). Once foals have been allowed to develop secondary complications, such as sepsis, the survival rate decreases. Early supportive care is key to treatment. Foals that have experienced a significant hypoxic injury are much more difficult to treat and can require the highest level of intensive care. Many foals can be managed successfully on the farm.
The main aims of treatment are to maintain hydration, provide nutrition, prevent sepsis, encourage maternal bonding and control seizures or other neurologic signs. It is important to maintain adequate tissue perfusion, which frequently involves the use of appropriate fluid therapy to restore and maintain circulating volume. Small boluses (20ml/kg) of isotonic crystalloids may be necessary to restore circulating volume in foals that are hypovolaemic. Many foals will then benefit from maintenance IV fluid therapy with 5% dextrose or another maintenance fluid (usually 3ml/kg/hr to 6ml/kg/hr). Inotropes and pressors may be necessary in more severe cases to maintain blood pressure and tissue perfusion.
Nutritional support is essential and the simplest way to provide this is via enteral feeding. Some foals may need some assistance to stand and latch on. However, many of these foals have a poor suck reflex and, consequently, may find it difficult to nurse from the mare and should not be fed from a bottle. The use of a small indwelling nasogastric tube can often be used to allow small, frequent feeding (Figure 4).
Enteral feeding should be monitored very closely as not all foals will tolerate large volumes of milk. A good initial target is 10% of bodyweight, which will provide maintenance fluid and energy requirements. Foals with more severe disease will not tolerate enteral feeding, therefore, parenteral nutrition and small trophic feeds will be required.

Most recumbent or severely affected foals will benefit from respiratory support. This is generally possible using humidified intranasal oxygen at 2L/min to 15L/min. Sternal positioning and encouraging mobility can also significantly improve lung function. Arterial blood gas analysis can be useful to monitor respiratory function. Foals with abnormal central control of respiration can also develop excessive hypercapnia (without hypoxaemia). In these foals the use of respiratory stimulants such as oral caffeine (10mg/kg PO followed by 2.5mg/kg PO q24h) or doxapram by continuous rate infusion can reduce hypoventilation.
Diazepam (0.1mg/kg IV to 0.2mg/kg IV) is usually the first choice drug to control seizures in the short term. However, the drug accumulates in tissue and is not suitable for long-term use. Midazolam by continuous rate infusion (0.02mg/kg/hr to 0.06mg/kg/hr) is an excellent choice when more prolonged treatment (6 to 72+ hours) is required. This drug has the advantage that the rate can be adjusted relatively easily and the medication can be discontinued without a prolonged effect. Phenobarbitone (2mg/kg to 10mg/kg by slow IV infusion up to q8h) reduces CNS excitability and can be used for the control of frequent, more severe seizures. The major downside of phenobarbitone treatment is its prolonged effect and significant respiratory depression.
Many other treatments have been proposed for NMS, but very little evidence is known to support their use. The use of antioxidants, such as vitamin E, C and thiamine, may help reduce oxidative damage. Magnesium sulphate has been suggested to prevent cellular death. No studies exist to evaluate its use in foals and studies from human medicine are conflicting. Dimethyl sulfoxide (DMSO), mannitol and dexamethasone have all been suggested to reduce cerebral oedema. Again, no studies exist in horses, and both mannitol and DMSO can create problems with osmolality.
Control and prevention of sepsis is absolutely critical. Foals should be checked for failure of passive transfer, and plasma administered if necessary. Broad-spectrum antimicrobial therapy should be considered in any foal judged to be at high risk of sepsis or showing any clinical signs of infection.

A great deal of interest exists in ways to reduce progestagen concentrations. However, it is still not known whether this is an appropriate way to try to accelerate recovery in these foals or whether a protective benefit may exist from the high levels of these compounds. Preliminary trials have investigated the role of drugs, such as dutasteride, to reduce progestagen production, but these are in their infancy and the appropriate drug and route of administration is not yet known.
A technique called “squeeze-induced somnolence”, or the “foal squeeze”, has been developed over the past few years to recreate the physical pressure of the birth process (Figure 5). The idea behind this technique is the physical pressure of foaling is an important trigger in reducing progestagen concentrations. In some foals this leads to a dramatic and rapid improvement in their clinical signs. This procedure can be easily carried out using a soft cotton rope. Further instructions can be found at https://bit.ly/2QK6uT7
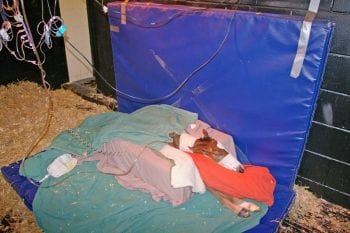
High standards of nursing care and hygiene are required. A quiet, warm environment, if possible close to the mare, is essential. Manual restraint on a padded bed to prevent self-inflicted trauma is important. Foals will need encouragement to rise, move, regain the suck reflex, interact with the environment, and finally nurse from the mare.
The prognosis for foals with NMS is usually very good with appropriate supportive care. Reported survival rates range widely, but can be as high as 80% to 90%. The prognosis for foals that experience significant severe hypoxic injury is generally poorer. Signs of uncontrollable seizures, anuric renal failure and severe cardiovascular dysfunction are generally associated with a poor prognosis.