21 Aug 2017
Andy Durham describes the advantages of using this diagnostic imaging technique when undergoing eye examination in horses.

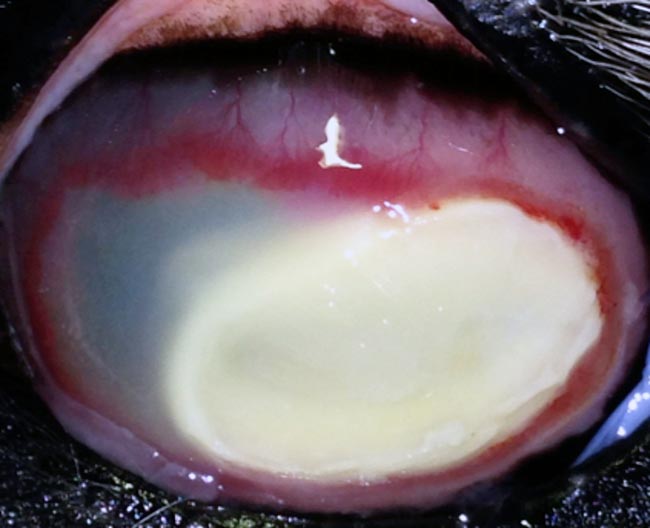
The use of ultrasound in eye examination is a simple and accessible, but greatly underused, technique, with many valuable applications in equine practice. The main indications for ultrasonography of the eye in horses is when deeper visualisation of the eye is impossible due to corneal opacity/oedema, opacity of the aqueous due to inflammation and/or haemorrhage (Figure 1), unresolvable miosis or an opaque lens.

Ultrasonography also offers a means of recording images of deeper ocular structures (such as lens abnormalities) for clinical records and provides a good indication of glaucoma in situations where tonometry is not available.
This brief discussion will provide common examples of where ocular ultrasound mightbe applied and reference information to facilitate interpretation.
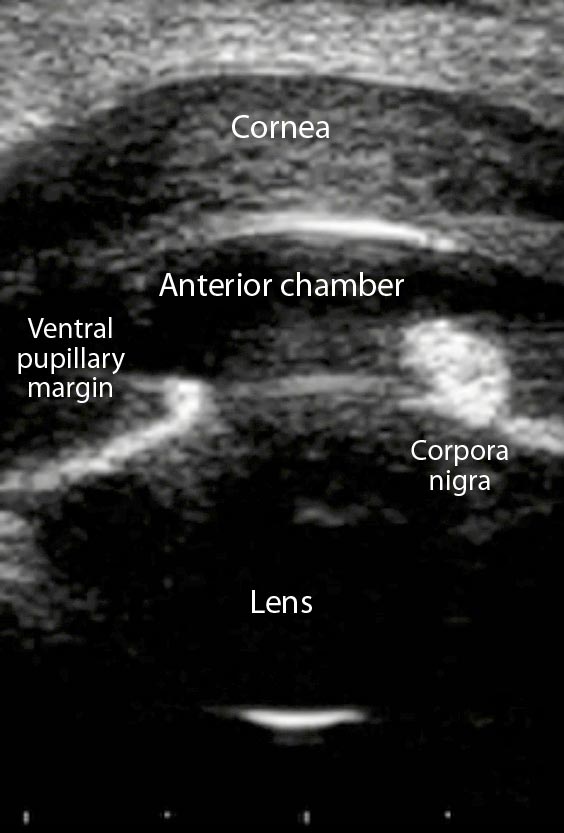
Ultrasonography is generally simple and easy to master, using standard orthopaedic or reproductive ultrasound equipment comprising a linear transducer, with between 7.5MHz to 12.5MHz frequency. Direct application of the transducer to the upper eyelid, to which standard ultrasound gel has been previously applied, will provide good images (Figure 2). A transcorneal technique is also described following topical desensitisation, but offers little advantage.
Nerve blocks are unnecessary, although the procedure is often greatly facilitated with the use of light sedation.

Generally, a horizontal plane (or at least parallel with the long axis of the pupil) is used for most images, but various angles might be useful for a thorough examination. Gentle pressure should be used to move the upper eyelid up and down, along with the transducer, for different image planes, initially attempting to obtain sagittal images.
Gentle pressure is needed to maintain a curved corneal surface, as slightly greater pressure will flatten the cornea and alter measurements of ocular structures.
The cornea, aqueous humour, iris, corpora nigra, ciliary body, aqueous humour, lens, vitreous, retina/choroid/sclera, optic nerve and retrobulbar space can all be visualised in virtually all horses.
It should be noted, though, that the normal equine lens will appear as a bright acoustic reflection from the rostral and caudal axial surfaces, with no further anatomic detail imageable in the absence of pathology (see further on).
Initial assessment of globe shape and size should reveal perfect symmetry in normal horses. When a good axial image is obtained, including lens reflections, the image can be frozen and the diameter measured. Most adult horse’s eyes are approximately 38mm to 42mm in diameter.
Bearing in mind it is possible to undermeasure, but not overmeasure, the diameter of a sphere, the globe diameter is taken as the largest of several measurements. Left and right globes should have identical diameters and not measure greater than 1mm different. Greater differences are supportive of glaucoma. Hypotonic eyes might also be detected following uveitis or structural injury to the cornea/sclera.
The cornea is easily imaged with focus settings very superficially. It has low echogenicity, with a bright reflection on the deep surface (Descemet’s membrane). The corneal thickness should be no more than 1mm in normal horses, but may be seen to be considerably thickened in some keratitis cases (Figure 3a).
This has important metabolic implications for a tissue that survives via diffusion of vital nutrients, and significant thickening should be aggressively countered with anti-inflammatory and osmotic agents.
The aqueous humour represents a totally anechoic area between the bright caudal corneal surface and the iris/lens (Figure 3b), and is approximately 3mm to 5mm deep. The presence of inflammatory debris, blood, fibrin and so on are very easily detected in comparison to the normal plain anechogenicity. This is especially useful for quantification and monitoring using previous recorded images for comparison over time.
The iris is a thin (2mm to 3mm) echogenic structure on the deep surface of the aqueous with a deeper peripheral echogenic ciliary body of up to 5mm thick with the combined structure extending from the peripheral sclera towards the lens.
Corpora nigra are easily visualised protruding from the iris into the aqueous (Figure 3b) and can occasionally create reverberation artefacts deep to the structures. Assessment of pupil size is a very important part of ocular examination, representing a cardinal sign of uveitis and iris spasm being a significant cause of ocular pain.
Where examination of the eye is difficult due to opacity, swelling or even severe blepharospasm, pupillary size can easily be measured with the transducer oriented vertically and the requirement for mydriasis determined (Figure 3b).
Smooth masses attached to the iris margins or corpora nigra generally represent benign and inconsequential fluid-filled cysts, although increased concern often arises in grey horses, where melanomata represent a differential diagnosis. Ocular ultrasound represents a quick and easy way of differentiating fluid-filled anechoic cysts from diffusely echogenic solid melanomata, with the additional advantage of accurate measurement of dimensions for further monitoring (Figure 4).
In the normal horse, the lens itself is anechoic, although small hyperechoic reflections are consistently seen on the axial anterior and posterior surfaces as the ultrasound waves transfer from aqueous to lens, and lens to vitreous perpendicularly to the ultrasound beam. Other than this, the normal lens should be featureless and between 10mm to 15mm thick (Figure 3b).
Cataracts are readily imaged with ultrasound, as increased echogenicity in particular areas of the lens with the lens capsule and nucleus easily distinguished (Figure 5). In fact, cataracts are often more clearly visualised ultrasonographically and the affected parts of the lens differentiated more easily than when using direct illumination or an ophthalmoscope. The additional benefit of easily recorded images also applies to ultrasonographic examination. The most common lens abnormality is nuclear sclerosis, which may be relatively normal in mature to ageing horses, and is generally well-tolerated. This is easily seen as a central spheroid echogenic structure within the anechoic lens.
Incipient cataracts are associated with echogenicity comprising less than 5% of the lens, immature cataracts comprise 5 to 95% lens echogenicity and mature cataracts have echogenicity occupying more than 95% of the lens.
Hypermature cataracts are associated with lens shrinkage, whereas intumescent cataracts are associated with abnormally increased lens size. Occasionally, lens rupture or dislocation might also be seen.
The vitreous should be anechoic in the normal horse and is typically 15mm to 20mm deep.
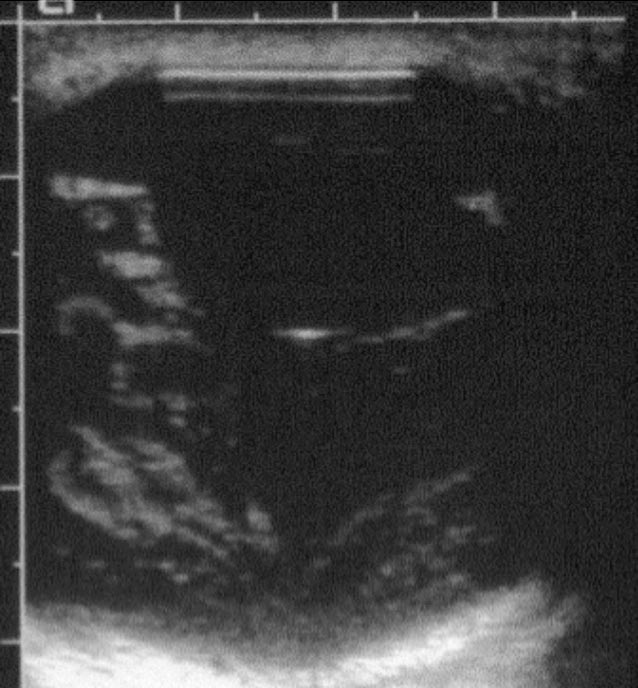
Abnormalities of the vitreous are readily visualised as diffuse, focal or membranous opacities, often mobile and swirling, and may represent haemorrhage, fibrin, inflammation, hyaloid vessels and so on.
This is often seen as part of uveitis/panophthalmitis (Figure 6) – although, occasionally, extensive vitreal opacity is seen in the absence of other ophthalmic changes.
It is difficult to see a distinct retina separate from the underlying choroid and sclera, and the combined structure is typically 2mm to 3mm thick. Total retinal detachment is readily identified with a typical “birds wing” appearance – although, occasionally, partial detachments might also be seen (Figure 7).
Other retinal concerns, such as melanoma or proliferative neuropathy, may also be better defined using ultrasound than ophthalmoscopy (Figure 8).
Where exophthalmos is seen in the absence of increased intraocular pressure or globe size (Figure 9), the examination of deeper retrobulbar structure is indicated. The optic nerve can be followed through the retrobulbar space, which has a conical structure decreasing in diameter as it leaves the back of the eye surrounded by retrobulbar fat.
Relatively anechoic extraocular muscles are also seen with a bright white echogenic line, representing the surface of the bone. Examination of the retrobulbar structure is definitely more challenging than examining the globe itself.
Often a sector probe with lower frequency (5MHz to 7.5MHz) is useful and frequent comparisons to the contralateral eye is helpful.