22 Feb 2022
The science behind early enteral nutrition and the practicalities of using this to improve patient outcomes.

Research is shedding ever more light on the importance of promoting food intake soon after surgery.
Here, we review the evidence-base for early enteral nutrition and discuss how best to provide nutritional support in the post-operative phase.
The evidence-base for early postoperative nutritional support is more developed in human medicine. In this field, it is reasonably well-accepted that early nutritional support decreases mortality as well as shortening the duration of hospitalisation1,2. In the veterinary sphere, research evidence is more limited, but a 2012 study of dogs with septic peritonitis found that initiation of consistent caloric intake within 24 hours of surgery was associated with a significantly shorter hospital stay3.
Nutritional support post-surgery can be delivered either enterally, or parenterally via the IV route. In human medicine, enteral nutrition is associated with shorter hospital stays, a lower infection rate and earlier gut function as compared to parenteral nutrition.4
Though there are some situations where enteral feeding is contra-indicated – for example, excessive vomiting, GI tract blockage or excessive GI haemorrhage5,6 – it should be attempted where possible as the provision of nutrients enterally has several physiological benefits. Firstly, by directly stimulating the GI mucosa, enteral nutrition causes the release of hormones that support the recovery of GI motility5. This will help counteract postoperative ileus, a common complication after surgery.
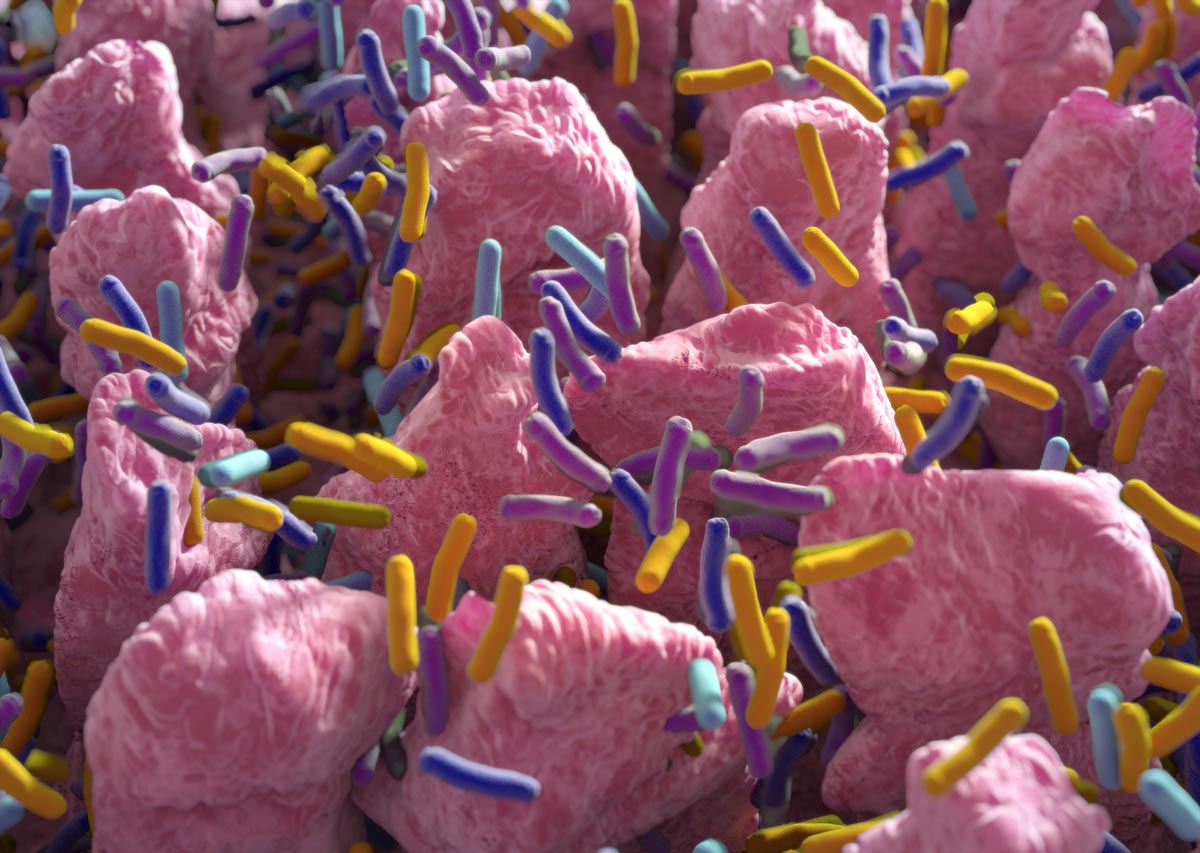
Secondly, enteral nutrition may help protect against bacterial translocation.5,7 When nutrition is not provided enterally, the lack of intraluminal nutrients is associated with decreased GI cell turnover and mucus production, impairing gut barrier function. This, coupled with reduced GI blood flow associated with lower luminal fill, can result in higher gut permeability, increasing the infection risk5.
Finally, enteral nutrition helps preserve a healthy gut epithelium. Studies in rats have shown villous atrophy within three days of the onset of total parenteral nutrition, illustrating the importance of intraluminal nutrients6. By preserving villous structure, enteral nutrition supports the body’s ability to absorb nutrients to aid recovery from anaesthesia and tissue trauma.
In the clinic, effective postoperative nutritional support depends on two main factors: selecting the right diet, and making sure the patient’s intake is sufficient to meet their needs. When considering diet type, it helps to identify the specific metabolic changes that occur in the recovery phase and consider how these relate to nutritional requirements.
Research on post-surgical recovery in human medicine suggests that in the first 24-48 hours, metabolic rate drops and blood flow to the gut is reduced. Given the low GI perfusion, it is a priority to initiate voluntary food intake to supply nutrients to the intestinal tract5,8,9. To encourage feeding, palatability is an important factor as many animals in the immediate postoperative period show some reluctance to eat5,10.
After the first 48 hours and up to 14 days post-surgery, the metabolic rate is increased8,9. This means that provision of sufficient energy is a key goal. A high level of protein is required, as this will be used for wound healing and the synthesis of acute phase proteins and immunoglobulins, as well as catabolised for energy. Diets should therefore have a high energy density and sufficient protein of high biological value. A highly digestible diet is also a priority given the likelihood of appetite reduction.
In addition, certain specific nutrients could potentially help shorten the recovery period. These include long-chain polyunsaturated omega-3 fatty acids, which have natural anti-inflammatory effects, as well as arginine which is known to promote wound healing. Glutamine and taurine are other key amino acids, and prebiotics such as inulin and fructo-oligosaccharides can provide support for the GI microbiome during recovery5.
GI diets, such as PRO PLAN® Veterinary Diets EN Gastrointestinal are appropriate for most healthy animals after routine surgery. In addition, probiotics such as PRO PLAN® FortiFlora® are often employed to provide additional support.

Depending on the clinical situation, some cases may require a different specialised diet. Critical care diets such as PRO PLAN® Veterinary Diets CN Convalescence can be useful for some patients with serious illness – these diets typically have an even higher energy density with fat providing the main energy source.
As well as selecting an appropriate diet, it is necessary to ensure the patient consumes enough of it. As a minimum, hospitalised patients should eat enough to meet their resting energy requirement (RER)10, which is defined as their energy needs at rest in a thermo-neutral environment and is calculated as follows:
RER = (body weight in kg)0.75 × 70 kcal of ME/d.
However, anorexia and hyporexia are common, especially immediately after surgery. To encourage hyporectic patients to eat, nursing care is key. Voluntary food intake can be encouraged in multiple ways, such as making sure the food is fresh (so only leaving it down for short periods of 20-30min), heating it to body temperature, and hand-feeding if this suits the patient. Catering to the patient’s food preferences in terms of dry or wet diets is also important, with texture being particularly significant for cats. Offering several options concurrently in a ‘buffet’ is now often advised against to reduce food aversions. Other elements of holistic care, such as providing adequate pain relief and making sure the environment is calm with a natural light-dark cycle, should also be factored in5,10.
If sufficient voluntary food intake cannot be encouraged, assisted feeding may be required, with the technique dependent on the clinical situation. Nutritional support post-surgery must always be tailored to the individual patient’s needs, but, as a general rule, factoring the importance of early enteral nutrition into post-operative plans will help clinicians improve patient outcomes.