13 Dec 2022

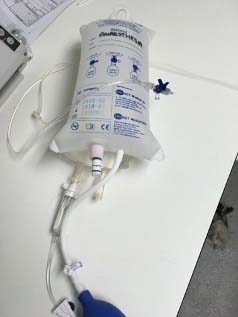
Figure 7. Use of negative pressure wound therapy in a cat.
The cause and severity of wounds are diverse, but the fundamentals of treatment remain to ensure the patient is stable, to identify all concurrent injuries, and to manage the wound to minimise contamination and provide protection for healing to begin.
An early complete clinical examination should identify life-threatening wounds – particularly those penetrating the abdominal or thoracic cavity. Analgesia (and possibly oxygen) should be provided early and emergency treatment of life-threatening problems (such as a pneumothorax) take precedence over the wound.
The aim of initial wound management is to reduce microbial and foreign material contamination.
Gloves – not necessarily sterile – should be worn for assessment and treatment of all wounds. Pack the wound with cheap sterile gel (no need for expensive hydrocolloid at this stage) and clip widely (Figure 1).
Imagine the wound as a surgical site and aim to clear all of the surface that a subsequent dressing will cover; this facilitates decontamination of the surrounding skin with antiseptic scrub, and hair carries around three times the amount of bacteria as clipped and cleaned skin.
It may be helpful to clip as though you were about to perform a surgery on that area – for example, the full hemithorax and length and circumference of the limb. The skin around the wound (the “peri-wound”) can then be prepared with chlorhexidine or iodine surgical scrub solution.
Subsequently, gross contamination can be removed from the wound using forceps and copious lavage (removing bacteria, debris and the gel). Potable tap water hosed or showered over the surface is fine for highly contaminated wounds, and can help reduce the microbial burden of the peri-wound as well – initially, volume is more important than sterility.
Once the site is clean, isotonic saline or lactated Ringer’s solution is generally accepted to be the best option to allow effective removal of bacteria and small particles without damage to fibroblasts. A pressure of 8psi is the aim – this is most consistently achieved with a 1L fluid bag, a giving set with the hub of a 21G needle attached and a pressure cuff at 300psi (Figure 2).
Any clearly devitalised tissue can be sharply debrided; however, if the status of the tissue is unclear, it may be more appropriate to leave it in situ until it declares itself viable or necrotic (assessed daily at first, and ischaemic necrosis usually occurs within the first five days).
Surgical debridement should be performed with aseptic technique, commonly in a clean preparation area, although for more serious wounds, potentially in an operating theatre.
Decision-making relies on wound, patient and owner factors, which are regularly reassessed to modify the overall plan for final healing.
From the first consultation, it is helpful that owners understand the unpredictability, the duration and the costs of treatment.
While the principles of immediate treatment are reassuringly consistent, ongoing management is expected to change according to progress in the phase of wound healing and volume of wound exudate. Unexpected changes result from a lack of progress in healing or developing complications (such as infection).
Closure can present challenges depending on the location and extent of the wound, and many options exist.
Some clean-contaminated, sharply incised wounds presented less than six to eight hours after injury may be candidates for pragmatic primary closure with sutures or staples, but essentially, a clear, thorough warning needs to be given to owners that this might not be successful – often as a result of subsequent ischaemic necrosis or infection.
Primary closure is unlikely to be successful for wounds with questionable tissue viability or those with large defects resulting in tension, although occasionally, large skin flaps can provide a temporary protection for underlying tissue – even if necrosis is predictable (Figure 3).

Delayed primary closure – prior to the formation of granulation tissue – facilitates better assessment of tissue viability in the first few days and improved decontamination of mildly contaminated or traumatised wounds. For more severely contaminated wounds, closure may be more successful after a period of open wound management and the development of granulation tissue – normally more than three to five days following injury in dogs, but generally longer in cats. Granulation tissue is highly resistant to infection and provides a vascular bed to improve healing potential.
With appropriate owner counselling regarding the timescale and commitment, second-intention healing can lead to a favourable outcome without the need for surgical intervention, even for quite large skin defects.
The resulting new epithelium is more fragile, but this is uncommonly a problem in small animals. Rapid contraction can occur around 7 to 14 days into healing, but all wounds then reduce slowly with reliant epithelial migration; large wounds can be closed after a period of second-intention healing, if necessary, by debridement of at the edge of epithelialisation and undermining or margins to eliminate tension.
Cicatricial contraction adjacent to mobile essential anatomy (for example, the eyelids) or across joints may mean that some locations are without mobile loose skin, meaning second-intention healing is not the most appropriate option, and either primary, delayed primary or secondary closure are more sensible.
Alternatively, restrictive scarring can be managed by reconstructive surgery if it is already developed.
Choice of dressing should be guided by the wound. Initially, they may be used to facilitate debridement. Subsequently, to maintain a moist environment (removing excess exudate, but providing moisture to dry wounds) promote optimal conditions for healing and protect the granulation bed during epithelialisation. The most appropriate dressing will, therefore, change throughout the treatment process as the wound healing progresses.
Contaminated acute or chronic wounds may benefit from a debriding dressing following lavage, but these are discontinued when gross contamination is managed. Wet-to-dry dressings can create a dry wound surface, are quite aggressive and are non-selective; they are used sparingly for obvious gross contamination and changed daily with good analgesia or general anaesthesia.
Autolytic debridement is gentler on cells (including the use of hydrocolloid gels and foams), but may not manage particulate foreign material as readily. Bactericidal dressings – such as materials soaked in hypertonic saline, honey or silver-containing products – can help limit infection, or surface contamination developing into infection.
Honey is hyperosmotic, and while it can reduce inflammation due to antioxidant production and stimulation of cytokine release, it can increase the volume of exudate and cause tissue maceration. It is most useful in the early inflammatory phase if concern exists regarding wound infection.
Wounds producing a low volume of exudate benefit from the addition of moisture in the form of a hydrocolloid gel covered by a semi-occlusive dressing. Options for more exudative wounds include polyurethane foam, which forms a gelatinous layer on contact with wound exudate, maintaining moisture. Heavily exudative wounds risk strike-through and then bacterial contamination through the dressing, and so a second highly absorbent layer on top (for example, a children’s nappy) or commercially available foam dressings with superabsorbers can be helpful. Negative pressure wound therapy devices are also excellent at removing exudate and have other beneficial properties in stimulating the development of granulation tissue in those wounds that need it.
The anatomical location of wounds can require a little creativity in keeping dressings in place. While those on areas of low movement are easily secured with adhesive dressing retention tape or a tie-over bandage, wounds near the mouth, eye, anus and so forth can be more difficult to cover.
Dressings can be attached directly to wound margins with sterile skin staples (Figure 4). Animals can rarely be trusted with dressings – an Elizabethan collar is important to prevent interference.
Many of the most recent developments focus on attempting to reduce the inappropriate use of systemic antimicrobials. The World Health Organization lists antibiotic resistance as one of the top 10 threats to human health and it is our responsibility to use antibiotics only where necessary.
Recent work has focused on how we can better identify infection to reduce blanket usage and investigated options other than systemic antibiosis. Most wounds encountered are contaminated (bacteria are present on the surface), but infection refers to the invasion and replication of microbes within the tissue itself. This distinction is important since contamination can be managed better topically rather than systemically.
The use of systemic antibiotics is controversial in wound management. Once granulation tissue has formed, the wound will be intrinsically resistant to infection and, if used initially, systemic antimicrobials should be discontinued.
The use of topical antimicrobials may reduce or eliminate the requirement for systemic antibiotic use – particularly where wounds are contaminated rather than infected – and may also be effective, even against antibiotic resistant strains of bacteria.
In-house cytology of the wound can be extremely useful in guiding the selection of a topical antimicrobial drug (rods may be susceptible to a combination of silver sulphadiazine and amikacin versus cocci, which may be susceptible to fusidic acid). Wound cytology also allows a semi-quantitative assessment of the extent of contamination and whether it may be developing infection, and to monitor the response of the area to treatment, or whether a change occurs in bacterial species since the initial injury.
It is quick, easy and cheaper than culture, although it does not replace wound tissue culture as the gold standard to identify infection and determine the most appropriate antibiotic if systemic therapy is necessary.
Topical antiseptics are preferable to antibiotics, since less risk exists of problematic bacterial resistance developing. A 2018 consensus statement described hypochlorous acid as a “first-choice agent for single or repetitive antiseptic cleansing of contaminated traumatic wounds”, and its effectiveness against colonisation with MRSA has been established.
These products are affordable, comfortable and can be applied by the owners at home to wounds in all phases of healing.
Other options include polyhexamethylene biguanide, which is available in liquid or gel form, and is an effective antiseptic for colonised and infected wounds.
A swab from the wound exudate or from the surface of the wound (particularly the acute wound) often represents contaminant species – particularly if several species are identified. Tissue cultures have a higher sensitivity and specificity than swabs in deeper human infections, and should be considered more reliable than a superficial wound swab.
To collect a sample for tissue culture, thorough lavage and debridement should be completed prior to sampling.
A section of tissue from the wound bed or margin can be sharply removed. It should be wrapped in a sterile saline-soaked swab and placed into a sterile container to prevent desiccation during transport.
On a similar theme, tools are being developed to identify the presence of infection. Currently, clinical assessment coupled with microbiology is the standard of care for determining likely clinically significant levels of bacteria.
The disadvantage of this is the subjective nature of assessment, potential sampling of non-infected tissue and the delay in receiving results from external laboratories.
The MolecuLight i:X device (MolecuLight; Canada; Figures 5 and 6) is a portable device designed to be used alongside clinical and laboratory assessment, and uses bacterial fluorescence to aid the identification of infection.
The ability to see actively respiring bacteria in real time may allow clinicians to more specifically localise infection within the wound bed to guide sampling to increase the diagnostic yield of cultures, better target debridement, and allow earlier cessation of antibiotic therapy.
Recent work with the device in human medicine has shown promise with management of burn wounds and traumatic military wounds. It has been established that most bacteria lie at the periphery of wounds – this may be a more reliable region for the tissue culture samples in the absence of a device.
The use of negative pressure wound therapy (NPWT) is longer established and relies on the local application of subatmospheric pressure on the surface of the tissue. NPWT is applied by placing a foam or gauze on to the wound, covered by an occlusive polyethylene sheet that seals the dressing.
A suction tube covers a perforating hole in the surface and either continuous or intermittent suction is applied – usually for three to seven days (Figure 7).

Literature is inconsistent as to the benefits of NPWT in different situations, but the authors have generally found rapid development of impressively healthy granulation tissue in the majority of cases.
Reported benefits include increases in wound perfusion, a reduction in oedema and the removal of exudate. Some studies have found a reduction in perfusion at higher pressures, so -80mmHg to -125mmHg is commonly used in companion animals, depending on the dressing applied.
Vascularity may be increased – wounds treated with NPWT may have an increased expression of vascular endothelial growth factor and interleukin-8, stimulating angiogenesis.
While NPWT alone will not treat wound infection, it may increase the resistance of the host to infection, and allows instillation of topical antiseptics through ingress catheters so that concurrent lavage is possible with the dressing in place.
Use beyond seven days can delay wound contraction.