13 Oct 2020

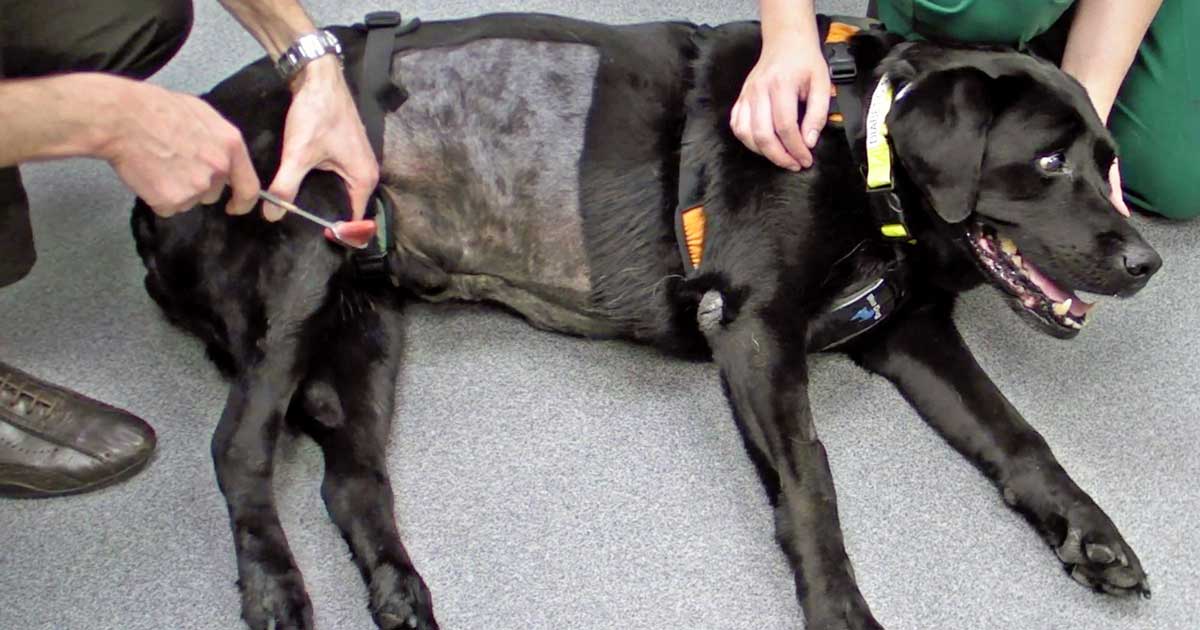
Figure 1. Patellar reflex. Image: Sebastien Behr
Part one of this article analysed the key information that needs to be collected from owners and explained the first steps of the neurological examination (behaviour and mental status, posture, gait and postural reactions).
Part two describes the key spinal reflexes, helps in localising the lesion, and examines how to properly assess nociception while also giving advice on prognosis depending on the neurological findings and their progression.
Spinal reflexes are segmental; therefore, they assess the reflex arc made by the limb’s sensory nerve, segmental spinal cord (C6 to T2 for the thoracic limb; L4 to S1 for the pelvic limb) and motor component. They do not assess communication to the brain; they are a local, unconscious reaction.
Spinal reflexes cannot be used for prognosis and their presence or absence should not be confused with the response to nociception (which should show a conscious response, such as turning the head or growling).
Spinal reflexes are either present or absent/weak. Exaggerated reflexes can be difficult and subjective to judge.
In cases of lesions to the sciatic nerve, the patellar reflex could be exaggerated because of the lack of resistance from the muscles in the caudal part of the leg and stifle. This is called pseudo‑hyperreflexia.
The most commonly tested spinal reflexes are patellar, flexor withdrawal, perineal and cutaneous trunci. Extensor carpi radialis and cranial tibial reflexes are also frequently tested. It is also important to assess muscle tone of the limbs before performing these tests.
Most tests are assessed in lateral recumbency and it is useful to start with the hindlimbs. It is also important to have the patient’s full cooperation for these tests, as they could voluntarily interfere with the response.
Cats may prefer to be held on their back, in a slightly seated position, for these tests.
Muscle tone is assessed by applying gentle pressure to the paw and testing the resistance. It can also be performed in a standing position.
In a normal dog, the limb should flex easily. If the extensor tone increases, it indicates an upper motor neuron (UMN) lesion. Decreased or flaccid muscle tone is suggestive of a lower motor neuron (LMN) lesion.
Patellar reflex is best tested in lateral recumbency. The thigh is held and the stifle is gently kept in a slightly flexed position.
The patellar ligament is struck with a reflex hammer, using the opposite hand. The stifle should extend quickly in a normal patient.
This reflex tests the integrity of the femoral nerve and L4 to L6 spinal cord segments. The femoral nerve is very important for holding the animal’s bodyweight.
Animals with an orthopaedic disease (such as cruciate disease or patellar luxation) or elderly animals may have reduced patellar reflex (Figure 1).
For the withdrawal (flexor) reflex, the skin between the digits is pinched – the animal should quickly and strongly withdraw the paw towards the body, flexing all the joints.
This test can be performed on all four limbs and it is important to compare the four legs.
The test assesses the spinal cord segments C6 to T2 (thoracic intumescence) and L6 to S2 (lumbar intumescence), and the nerves originating from these segments.
If a lesion of the sciatic nerve is present (for example, due to a foraminal stenosis), the animal will flex the hip, but not the stifle and hock joints.
If the animal shows a behavioural reaction (such as turning, biting or whimpering) when the digits are being pinched, this shows integrity of the nociception (or deep pain sensation).
As a general rule, an animal that is able to walk or move the legs should have intact nociception, especially if a spinal lesion is suspected.
When testing the withdrawal reflex, if the animal extends the opposite leg, it is an indication of a UMN lesion typical of chronic myelopathies. This is defined as a pathological reflex.
This reflex happens naturally in a standing position when one leg is lifted, to redistribute the bodyweight to the other leg, but it should be absent in a recumbent animal.
With the perineal (anal) reflex, the anal sphincter contracts and the tail flexes when the perineum is gently touched or pinched.
This reflex assesses the spinal cord segments S1 to S3 and the branches of the pudendal nerve. It is an important test in animals that have urinary incontinence. It is also useful to observe the anal tone before testing this reflex.
In animals with severe L6 to S2 LMN spinal cord lesions, the anal tone could be lost and the perineal reflex absent.
The cutaneous trunci (panniculus) reflex should be tested with the patient in an upright position. The skin lateral to the spine should be pinched, starting cranially to the lumbosacral region and moving cranially, one segment at the time. This should be performed on both sides. The skin should contract when pinched.
This reflex is present only in the thoracolumbar region. If a cut-off of contraction occurs (the skin stops contracting when pinched), this indicates a spinal cord lesion one to four segments (two vertebrae) cranially to the cut-off.
This test assesses the sensory integrity of the dermatomes and their spinal cord segments, and of the lateral thoracic nerve (efferent branch) and the C8 to T1 spinal cord segments.
A lesion of the brachial plexus may affect the lateral thoracic nerve, giving an absent cutaneous trunci reflex along the same side of the lesion.
This test is mainly used to help localise the lesion in the T3 to L3 spinal cord segment.
Light palpation should be performed first and it helps detecting swelling, deformity or abnormal range of motions.
Deeper palpation helps detect areas of pain. It is useful to palpate the whole spine, cranial to caudal. The thoracolumbar spine can be palpated by pressing between the spinous processes of the vertebrae and the paraspinal muscles, firstly gently then slightly more deeply. It is recommended to support the animal ventrally when palpating the spine.
When palpating the cervical spine, it is best to palpate the lateral processes first – if no pain is elicited, flexion/extension and lateral movements can be gently carried out. The tail can be also flexed and extended (Figure 2).

Spinal reflexes should be evaluated with the gait and postural reactions, to allow a more precise lesion localisation within the spinal cord.
After performing these tests, clinicians should be able to localise the lesion as cranial to T3 or caudal to T3, then either UMN (abnormal gait, postural reactions and normal reflexes) or LMN (abnormal gait, postural reactions, reduced muscle tone and abnormal reflexes), within these two areas.
As general rule, a lesion that affects the spinal cord C1 to C5 should give UMN signs to the thoracic and pelvic limbs, a lesion C6 to T2 should give LMN signs in the thoracic limbs and UMN signs in the pelvic limbs, a lesion T3 to L3 should have normal thoracic limbs and UMN signs in the pelvic limbs, and a lesion L4 to S1 should have normal thoracic limbs and LMN signs in the pelvic limbs.
Presence of LMN signs in all four limbs should raise the suspicion of a neuromuscular disorder (nerve/junction/muscle).
Exceptions to this rule are animals with severe peracute lesion of the thoracolumbar (T3 to L3) spinal cord. Although these animals should show UMN signs in the pelvic limbs (and, therefore, normal spinal reflexes), they present with hypotonia and absent spinal reflexes in the pelvic limbs (LMN signs). These signs may last for a few days after the onset of the clinical signs. This is called spinal shock in human medicine and its causes are poorly understood.
It is very important in non-ambulatory patients to assess the nociception, to ensure the pathways (spinothalamic tract) carrying pain sensation are still intact within the spinal cord.
These neurons lie deeply in the spinal cord; therefore, they are affected only by severe damage to the spinal cord. Nociception is an important prognostic factor in these patients.
The nociception is tested by pinching the animal’s digits or tail with the fingers first, and with a haemostat if no response occurs. Increasing pressure should be applied if no response occurs, and all the digits and legs should be tested for comparison.
In the pelvic limbs, it is important to test both medial and lateral digits, as the femoral nerve innervates the medial digits and the sciatic nerve the lateral digits. Nociception of the tail and perineum should also be tested, especially in animals where a L7 to S3 lesion is suspected.
An animal with intact nociception should react by showing awareness of the pain – turning the head, crying, trying to bite and trying to move away with the whole body are signs of intact nociception.
Nociception is a behavioural response of the patient to a painful stimulus. Withdrawal of the limb is not a sign of intact nociception, but only of an intact segmental reflex. Animals with severe UMN lesions may have intact withdrawal reflex and absent nociception.
It is useful to look at the animal’s head when testing the nociception – not the legs – as well as testing non affected limbs (Figure 3).

Clinicians should be able to provide an idea of prognosis to the owners of animals with a spinal cord lesion, based on the neurological findings and clinical suspicion.
It is very important to inform the owners about prognosis, as this can have a huge impact on their choices and expectations. It is also key to warn owners that the nervous system may take weeks and even months before recovering from damage, and that full function may not be always obtained.
The best way to provide owners with a more accurate prognosis is, of course, to investigate the exact cause of the neurological signs. Radiographs, MRI scans, electrodiagnostic tests, CT scans, CSF tap and blood tests are very useful to help clinicians reach a diagnosis in most cases. Lesion localisation and differential diagnosis should guide the choice of the most appropriate tests to perform.
Prognosis depends on several factors, including lesion localisation, the extent of the lesion and the suspected cause. For example, cats with urinary incontinence due to tail avulsion have a more favourable prognosis if anal tone and perineal sensation are intact on initial examination.
The onset and progression of the lesion can have an impact on prognosis. A slowly progressive lesion that is suspected to be neoplastic or degenerative could carry a poor prognosis, while more acute lesions that show signs of improvement (although often slowly) could have a more favourable prognosis, as a vascular cause is be suspected.
The clinical signs are very important, as signs such as absent nociception carry a poor prognosis. As general rule, animals with a suspected extramedullary compression that have absent nociception for more than 48 hours have a poor prognosis, even if the cause of compression is surgically removed. It is, therefore, very important to assess nociception with accuracy.
Animals that have a spinal trauma (fracture, luxation) and absent nociception have a very poor prognosis for recovery of function of the spinal cord, even if the fracture is reduced and stabilised soon after the trauma.
Animals with spinal cord compression for longer than five to seven days will take longer to recover after surgical decompression, especially if clinically non-ambulatory, and the functional recovery may not be complete.