6 Jun 2016

Figure 4. Abdominal ultrasonography of a six-year-old Tibetan terrier demonstrating the pancreas to be swollen and hypoechoic, and the surrounding fat to be hyperechoic, consistent with acute pancreatitis.
Acute gastrointestinal (GI) signs in cats and dogs can sometimes be challenging to manage. Medical history, physical examination and basic investigation, such as bloodwork, will often provide enough information to classify the clinical signs as primary GI or secondary to an extra-gastrointestinal condition.
Once an underlying extra-gastrointestinal condition has been ruled out, the clinician should assess the severity of the clinical signs and decide an appropriate diagnostic and therapeutic approach.
Uncomplicated GI signs can initially be treated symptomatically with dietary modification, antacid medication and antiemetic drugs as necessary. In the event of non-resolution or relapse of the clinical signs, or if the patient initially presents with certain criteria, including extreme age, depression, dehydration, hypothermia, marked pyrexia, cardiovascular instability, GI bleeding and abnormal abdominal palpation, further investigations and/or specific management have to be considered.
Abdominal ultrasonography and/or abdominal radiography will be necessary in some patients to provide a definitive diagnosis and rule out surgical disease.
Acute onset gastrointestinal (GI) signs are a common reason for presentation to veterinary practice. Although very common, acute vomiting and/or diarrhoea in cats and dogs can be challenging to manage.
Unfortunately, it is very difficult, and often impossible, to get a definitive diagnosis based only on clinical assessment and basic investigation. The aim of the first consultation in a dog or cat with acute vomiting and/or diarrhoea is to recognise which case needs immediate investigation and management, and which can be started on symptomatic treatment only and re-evaluated if no improvement is reported.
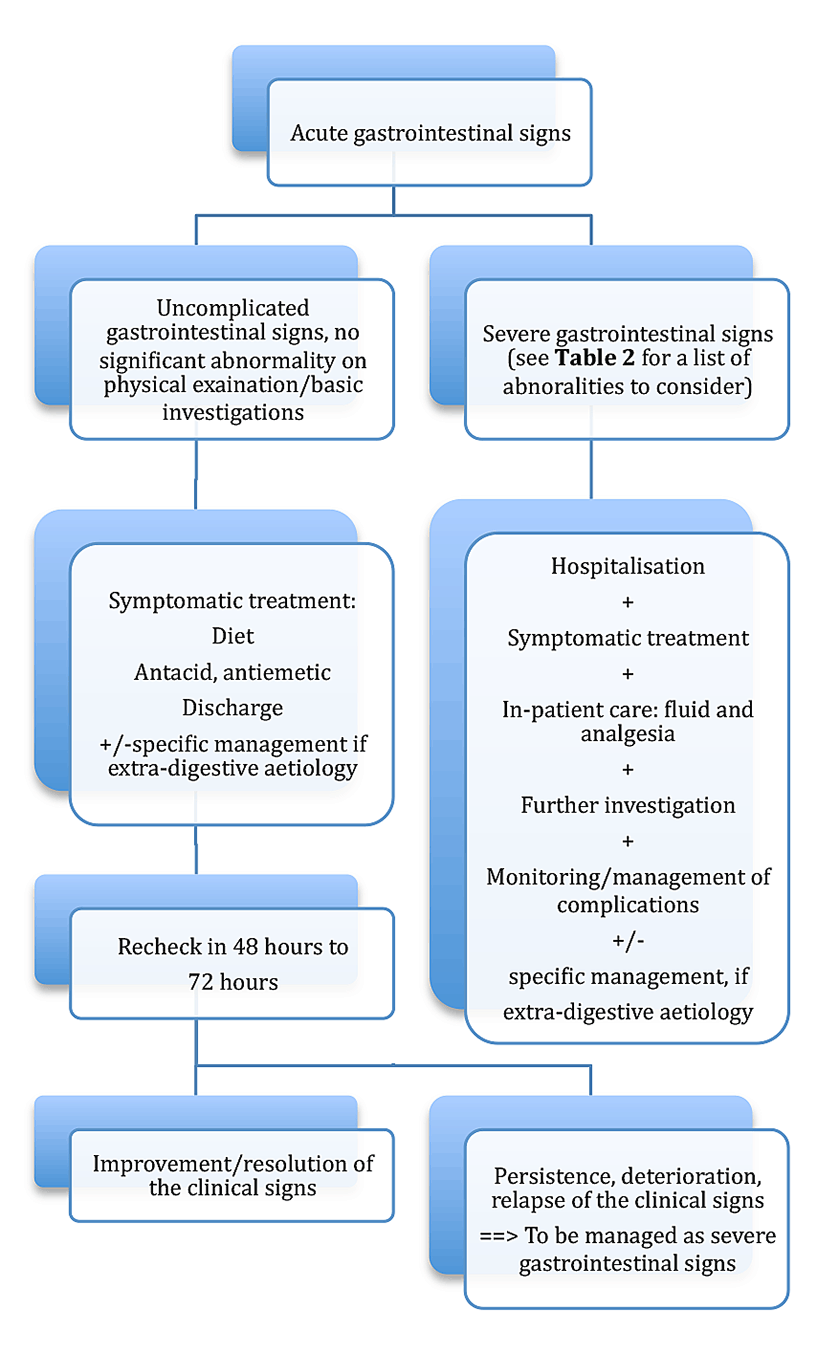
Identification of various abnormalities, including severe dehydration and hypovolaemia and melaena, will help the decision-making process (Figure 1). The differential diagnoses for acute GI signs are presented in Table 1.
| Table 1. Differential diagnoses for acute vomiting and/or diarrhoea in cats and dogs | ||
|---|---|---|
| Digestive | Infectious | • Bacterial: Salmonella, Campylobacter, Clostridium, pathogenic Escherichia coli and Yersinia. • Viral: canine distemper virus, canine parvovirus, feline panleukopenia virus, feline enteric coronavirus, FIV and FeLV. • Parasitic: helminth and protozoan. |
| Inflammatory | • Acute on chronic enteropathy: antibiotic responsive diarrhoea, diet responsive diarrhoea or inflammatory bowel disease. • Haemorrhagic gastroenteritis. • Gastric and/or intestinal ulceration. |
|
| Neoplastic | Gastric or intestinal tumour: carcinoma, round cell tumour and sarcoma. | |
| Obstructive | • Foreign body and partial/complete obstruction. • Volvulus. • Neoplasia. • Intussusception. |
|
| Diet | Dietary indiscretion and rapid dietary change. | |
| Drugs | Non-steroidals, chemotherapy and antibiotics. | |
| Extra-digestive | • Hepatobiliary disorders • Pancreatitis • Nephropathy • Endocrinopathy: hypoadrenocorticism, hyperthyroidism and diabetic ketoacidosis • Reproductive and urinary tract disorders: pyometra, prostatitis and orchitis • Miscellaneous disorders: CNS, disorders and drugs. |
|
A thorough medical history has to be taken, with particular focus on the duration and nature of the clinical signs. Diarrhoea and vomiting are considered acute if the duration is less than three weeks; however, the approach to a dog vomiting regularly for 24 hours may be different for a dog vomiting infrequently for two weeks.
It is important to ask the owner about his or her pet’s appetite, demeanour and thirst, and to characterise the nature of the faeces (melaena, haematochezia, mucus and frequency of defecation) and vomitus (blood, bile, undigested food, time lapse between the meal and vomiting and frequency of vomiting).
Differentiating between vomiting and regurgitation is of paramount importance. Regurgitation usually happens soon after eating – although it can sometimes be delayed and occur a few hours after eating, is not associated with abdominal effort, contains undigested food and is not associated with other signs relating to nausea, such as hypersalivation and gagging. This distinction is important, as the diagnoses and approaches are very different between regurgitation and vomiting.
Very young and geriatric patients are at particular risk of dehydration and rapid deterioration, and caution is recommended when managing them. Young patients have a higher risk of developing infectious gastroenteritis (for example, parvovirus – especially if their vaccination history is incomplete) and ingesting foreign objects.
A thorough physical examination should be performed, but particular attention should be paid to body condition score, presence or absence of dehydration, presence or absence of hypovolaemia, pallor or jaundice of the oral mucous membranes, abdominal palpation, rectal examination and rectal temperature.
Poor body condition, dehydration, hypovolaemia, pyrexia, pale/jaundiced mucous membranes, abnormal abdominal palpation (such as pain, mass and ascites), and GI bleeding (such as melaena, haematochezia and haematemesis) raise significant concern and their presence requires specific management.
Complete blood cell count or PCV measurement and blood smear evaluation, serum biochemistry – including total solids, albumin, urea, creatinine, liver enzyme activity bilirubin, cholesterol and glucose – and electrolyte measurement are part of the basic laboratory work-up.
These are recommended to exclude severe underlying conditions and/or secondary systemic consequences of a disease requiring specific management.
Parvovirus PCR on faecal material should be included in the diagnostic panel in suspicious cases, such as those involving young animals, incomplete vaccination protocol, haemorrhagic vomiting and/or diarrhoea and neutropenia.
Once a thorough history has been obtained, a detailed physical examination has been performed and basic investigations completed, the patient can be classified as having either uncomplicated or complicated GI signs, depending on the presence of severe abnormalities (Table 2). The former can be managed symptomatically, whereas, in the case of the latter, further investigations and/or specific management are deemed necessary.
Faecal culture is not commonly recommended in cases of acute gastroenteritis. Bacterial diarrhoea in dogs and cats is uncommon, and the presence of bacteria in a faecal sample does not necessarily mean this bacteria is causing the clinical signs. However, if there are immune-suppressed people in the household and zoonosis is a concern, faecal culture should be performed. Pathogenic Escherichia coli, Salmonella, Campylobacter, Yersinia and Clostridium (difficile and perfringens) are the most commonly identified bacteria.
| Table 2. Abnormalities characteristic of “severe” gastrointestinal signs | ||
|---|---|---|
| History/signalment | Physical examination | Basic investigations |
| • paediatric/geriatric patient • marked lethargy |
• dehydration • hypovolaemia • melaena • pallor/jaundice of the mucous membranes • cardiovascular instability • pyrexia • abnormal abdominal palpation • dyspnoea |
• anaemia • neutropenia • thrombocytopenia • azotaemia • hypoglycaemia • hypoproteinaemia • hyperbilirubinaemia • electrolyte disturbance |
Extra-digestive causes of vomiting and diarrhoea need to be identified as they can be addressed specifically. Basic investigations, physical examination and history are often enough to raise concerns for an extra-digestive cause of clinical signs.
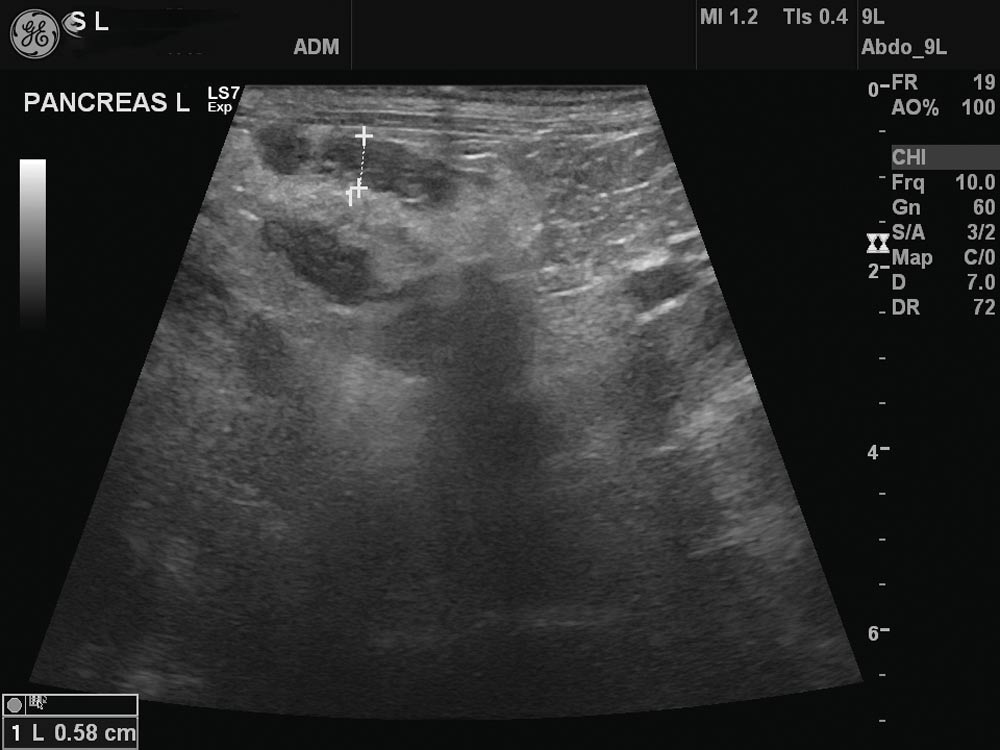
The clinical signs of pancreatitis are non-specific, ranging from a mildly reduced appetite to hypovolaemic shock, systemic inflammatory response syndrome, multiple organ dysfunction syndrome and death.
The absence of abdominal pain does not rule out pancreatitis and sensitivity of canine pancreas-specific lipase and feline pancreas-specific lipase is around 80% – a false-negative result is seen in approximately 20% of cases. A negative test result does not rule out pancreatitis.
Abdominal ultrasonography is often necessary to confirm the diagnosis, but imaging can be normal in acute pancreatitis.
Azotaemia is sometimes difficult to interpret in cases of vomiting and diarrhoea, as the azotaemia may be prerenal in origin rather than reflecting true parenchymal injury. Moreover, GI bleeding can lead to elevated urea when the glomerular filtration rate is not reduced.
Measurement of the urine specific gravity (USG) before starting fluid therapy can help differentiate between prerenal and renal azotaemia, as prerenal azotaemia is often characterised by a high USG (>1.040). Persistence of azotaemia after correction of hypovolaemia and/or dehydration, or severe azotaemia on presentation, raises a concern for a renal disorder. Differential diagnoses for acute kidney injury (AKI) include leptospirosis, cutaneous and renal glomerular vasculopathy (“Alabama rot”), pyelonephritis and intoxication. In many cases, the aetiology of AKI remains unknown.
Vomiting, diarrhoea, GI bleeding, hypovolaemia, absence of “stress leucogram” in a sick patient, hyperkalaemia and hyponatraemia raise concerns for hypoadrenocorticism.
It is important to remember the absence of electrolyte disturbances does not rule out glucocorticoid deficient hypoadrenocorticism. Basal cortisol should be used as a screening test for glucocorticoid deficiency. A value above 55nmol/L can be used to rule out hypoadrenocorticism, but a lower concentration does not confirm hypoadrenocorticism, and, in that case, an adrenocorticotropic hormone stimulation test is necessary. An addisonian crisis is life-threatening, and needs to be recognised and specifically addressed.
Other extra-digestive causes of acute GI signs, such as hepatobiliary disease, can be suspected based on bloodwork. These and other extra-digestive conditions require specific management and information can be gathered from other sources. In addition to specific management, GI signs also have to be addressed.
Cats and dogs presenting with a short history of diarrhoea and/or vomiting, without any concerning historical features, and with normal physical examination and bloodwork, can initially be managed symptomatically. The main differential diagnoses would include dietary indiscretion, parasitism or gastroenteritis of unknown origin.
A temporary diet change to a “highly digestible” or GI food is often recommended for five days to seven days. In cases of acute vomiting, a 12-hour period of starvation is recommended before reintroducing food, with a “little and often” approach.
The normal diet can then be gradually reintroduced once the clinical signs have resolved.
If the patient has not been wormed recently, a three-day course of fenbendazole (50mg/kg sid PO) is recommended. This has a broad spectrum and will act on ascarids, hookworms, whipworms, tapeworms, dipylidium and giardia.
Antacids, such as cimetidine 5mg/kg bid to tid PO, or proton pump inhibitors (omeprazole, 1mg/kg sid PO: used under the cascade) can be prescribed for a week in case of vomiting and/or nausea.
Antiemetic medication can be prescribed for a maximum of five days. Maropitant (1mg/kg sid SC or 2mg/kg sid PO) is usually recommended as it is licensed and its effects are limited to the CNS only, whereas metoclopramide also acts as a GI prokinetic and is contraindicated if GI obstruction or perforation has not been excluded.
Antibiotics are not recommended in the management of uncomplicated GI signs, as bacterial gastroenteritis is very uncommon in small animals.
Although case management requires modification to each situation, re-evaluation within 48 hours to 72 hours is usually recommended. If the clinical signs have improved, treatment can be continued until complete resolution.
However, if after two days to three days of treatment clinical signs have not improved, if new clinical signs have developed, or if the patient deteriorates in any way, further investigations are required.
The presence of one or more of the abnormalities detailed in Figure 1 should motivate further investigation and adequate treatment.
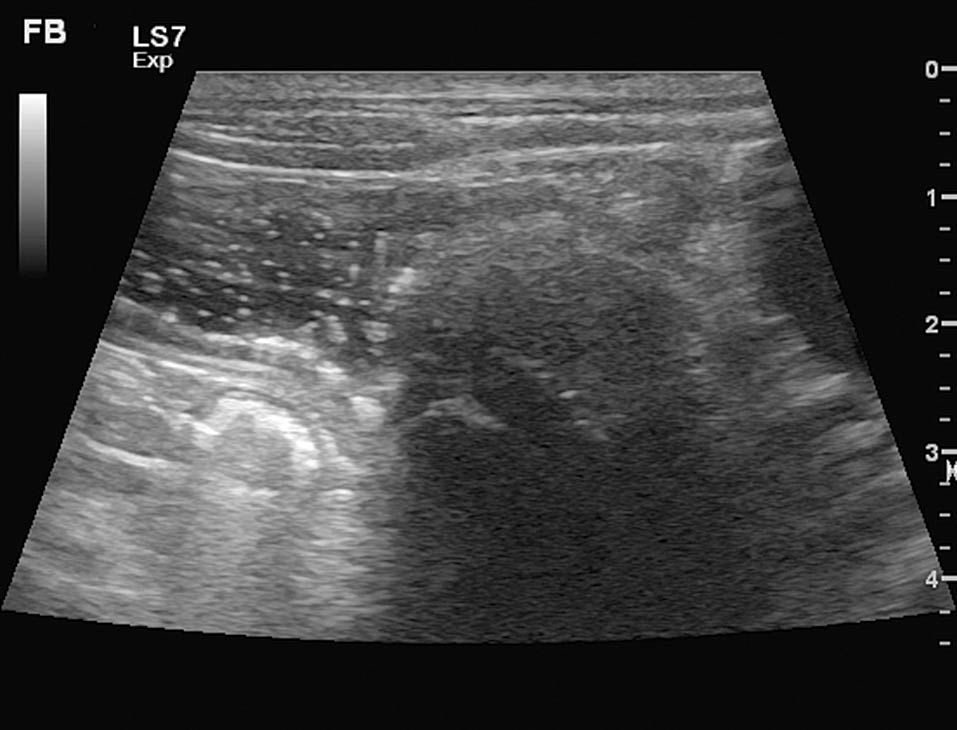
Imaging of the abdomen is performed to identify a potential cause for the GI signs.
Radiographic examination of the abdomen is a valuable and readily available technique, which may reveal major abnormalities including abdominal masses, foreign bodies and abdominal effusion.
However, abdominal ultrasonography is often needed to complement radiography, whenever there is a doubt about the diagnosis. Contrast radiography is infrequently helpful.
Ultrasonography of the abdomen is an incredibly useful tool for investigating abdominal disease and, in most cases, is far more sensitive than radiography. However, it is operator and equipment-dependent.
Examination can allow detection of partial or complete intestinal obstruction by a foreign body (Figure 2), intussusception (Figure 3), the presence of a mass lesion, non-specific changes associated with gastroenteritis of unknown origin (such as corrugated small intestinal loops and generalised ileus), and thickening of the small intestinal loops wall and/or gastric wall – consistent with neoplastic or inflammatory disease), as well as extra-digestive abnormalities such as pancreatitis (Figure 4).

Exploratory laparotomy would ideally always be performed once a surgical indication has been confirmed by ultrasonography. Exploratory laparotomy is unnecessary in most cases of acute gastroenteritis, except for obstruction, and can lead to deterioration in the patient’s clinical condition.
Abdominal CT is sometimes recommended when a patient’s size (above 40kg) makes satisfactory ultrasound examination difficult.
Depending on the results of bloodwork and imaging, other tests may be necessary for a definitive diagnosis. Endoscopy is usually not indicated in the diagnosis of acute GI disease, unless there is a suspicion of acute on chronic enteropathy.
Treatment of complicated gastroenteritis, including diet change, antacid and antiemetic medication, may be as for acute uncomplicated gastroenteritis, but this may not be adequate when the patient is presented with clinical signs such as dehydration, hypovolaemia, abdominal pain, pyrexia, or when basic investigations reveal anaemia, leukopenia, hypoalbuminaemia, electrolyte disturbance or other significant abnormalities.
Along with specific treatment, depending on the imaging findings and the other investigations, dehydration and hypovolaemia are recommended.
Dehydration is depletion of whole body fluid, while hypovolaemia refers to a decreased volume of fluid in the vascular system. Hypovolaemia and dehydration are not mutually exclusive, nor are they always linked.
Hypotension may exist separately or with hypovolaemia and dehydration. Fluid therapy is paramount in the management of hypovolaemia and/or dehydration and it is important to differentiate between these, as fluid therapy has to be delivered in different ways (Table 3). Crystalloids are usually indicated – using Ringer’s lactate solution 0.9% – for initial resuscitation.
Colloids may be indicated if the patient is hypoalbuminaemic, and/or if they remain hypotensive despite crystalloid boluses. Once hypovolaemia has been corrected, electrolyte disturbances, especially hypokalaemia, should be corrected by supplementing the crystalloid fluid.
Many diseases, such as acute gastroenteritis and pancreatitis, can cause abdominal pain. Due to the absence of contraindications and the good level of analgesia they provide, opioids are the best choice to manage abdominal pain, such as buprenorphine 0.01mg/kg to 0.02mg/kg IV every six hours to eight hours or methadone 0.1mg/kg to0.3 mg/kg every three hours to six hours.
In cases of severe and refractory pain, lidocaine and fentanyl can be given as constant rate infusions:
Antibiotics are generally only recommended in patients with neutropenia, or if there is a risk of bacterial translocation through impaired intestinal wall – especially if there is evidence of GI bleeding. In those cases, a broad-spectrum antibiotic is recommended, such as potentiated amoxicillin (amoxicillin and clavulanate, 20mg/kg IV tid).
Once an extra-digestive aetiology has been excluded, and if abdominal ultrasound is unremarkable or shows evidence of non-specific gastroenteritis, the treatments mentioned previously can be instituted for a few days. If GI signs persist for more than two weeks to three weeks, despite symptomatic management, or if they relapse, they are considered as chronic and require further investigations. Management of chronic GI signs will be discussed in the second article.
Once initial therapy has been started, such as fluid therapy and analgesia, frequent reassessment and treatment plan modification are important. Clinical signs can improve significantly in a short time frame, but complications can develop and have to be recognised and addressed rapidly.
Complications of vomiting and/or diarrhoea include dehydration, hypovolaemia (Table 3), electrolyte imbalance, acid-base disturbance, aspiration pneumonia, and malnutrition and/or protein depletion.
| Table 3. Assessment and management of dehydration and hypovolaemia | ||
|---|---|---|
| Dehydration | Hypovolaemia | |
| Causes | • Water loss (vomiting, diarrhoea and polyuria). • Reduced water intake (anorexia and adipsia). |
• Severe dehydration. • Rapid fluid loss (gastrointestinal losses, blood and polyuria). • Vasodilation. |
| Clinical signs | • Less than 5%: minimal loss of skin turgor, semi-dry mucous membranes and normal eye. • 7% to 8%: moderate loss of skin turgor, dry mucous membranes, weak rapid pulses and enophthalmos. • 10%: considerable loss of skin turgor, severe enophthalmos, tachycardia, extremely dry mucous membranes, weak/thready pulses, hypotension and altered level of consciousness. |
Mild/moderate: • Tachycardia. • Pink mucous membranes. • Normal to bounding pulses. • Short capillary refill time.Severe: • Bradycardia. • Pale mucous membranes. • Weak to absent pulses. • Prolonged capillary refill time. • Abnormal mentation. • Cold extremity temperature. |
| Management | To be corrected between 12 hours to 24 hours by crystalloid constant rate infusion. Calculation: Bodyweight (kg) x (per cent of dehydration/100) = volume (L) to correct in 12 hours to 24 hours + maintenance volume (2ml/kg) + ongoing losses (diarrhoea, vomiting and polyuria). |
• To be corrected rapidly by crystalloid boluses. • 10ml/kg to 20ml/kg in 10 minutes to 20 minutes for dogs and 5ml/kg to 10ml/kg in 15 minutes to 20 minutes for cats, to be repeated until cardiovascular status is more stable (resolution of tachycardia, normotension and improved demeanour). • To be modified (reduced) if cardiac condition suspected of anuria/oliguria. |
Should GI signs persist and/or the animal deteriorate, referral may need to be considered, as more intensive medical management and further tests, such as specialist ultrasonography and/or endoscopy, may be necessary.