19 Jan 2022

One of the major challenges in performing a neurological examination in cats comes from the fact they are not very cooperative within a veterinary clinic.
Dogs are usually more than happy to move and walk around with owner guidance, whereas even the most compliant cat is often reluctant to walk around the consult room to “show off” its moves.
The neurological assessment in cats is also often limited in time due to their non‑cooperative nature – hence assessment of a few key tests is far more important than performing a barrage of tests that are more than likely to result in an angry cat.
This article will give tips on determining when a cat has a neurological problem, followed by specific aspects of the neurological examination that can help in diagnosing the condition causing those clinical signs.
Therefore, even when your cat is as uncooperative as a tiger, you can still glean something from the advice given here.
Before embarking on a neurological examination, it is important to determine whether a neurological exam is the right thing to do. Many cats present with clinical signs that can mimic neurological disorders and so performing neurological examinations in these patients can be misleading if a general clinical examination is not performed first.
The aims of the neurological examination are to answer the following questions:
Having performed a general clinical examination, gait analysis is also very helpful in determining whether a cat has a neurological condition (see below).
The third question can be answered by collating information obtained in history taking with the neuroanatomical diagnosis and the patient’s signalment to compile a list of likely differential diagnoses.
Disease severity is obtained by performing specific components of the neurological examination – and this will determine the eventual prognosis of the conditions named on the differential diagnosis list.
Probably the single most important aspect of any examination is the opportunity to observe the cat moving around – and this presents the first challenge in assessment.
Most cats are sedentary and prefer to laze around with only short bursts of activity during the day. Therefore, many cats will be reluctant to move – regardless of their health – during a short consultation.
Alternatively, other cats are so traumatised by their visit to the vet that they will rush out their basket and hide in the smallest space in the room, preventing assessment.
The best way to counteract this is to ask the owners to obtain video footage of their cat’s activity at home, displaying any of the owner’s concerns on their smartphone. Therefore, any lameness, weakness or incoordination can be easily detected without upsetting the patient.
Three abnormalities can be assessed during gait analysis:
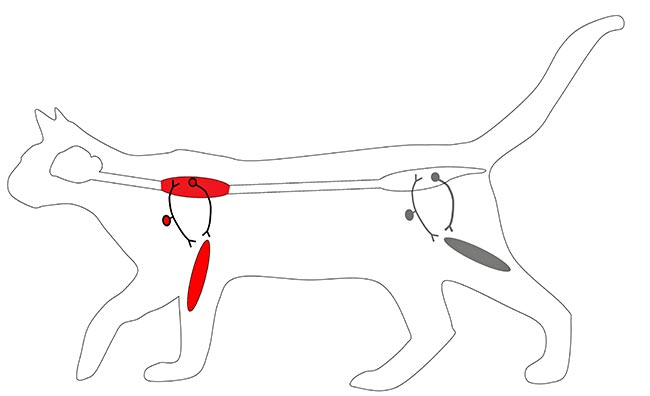
Paresis is defined as weakness or an inability to generate a gait.
The term paresis implies some voluntary movement is present, as compared to paralysis (or -plegia) in which complete loss of voluntary movement is observed.
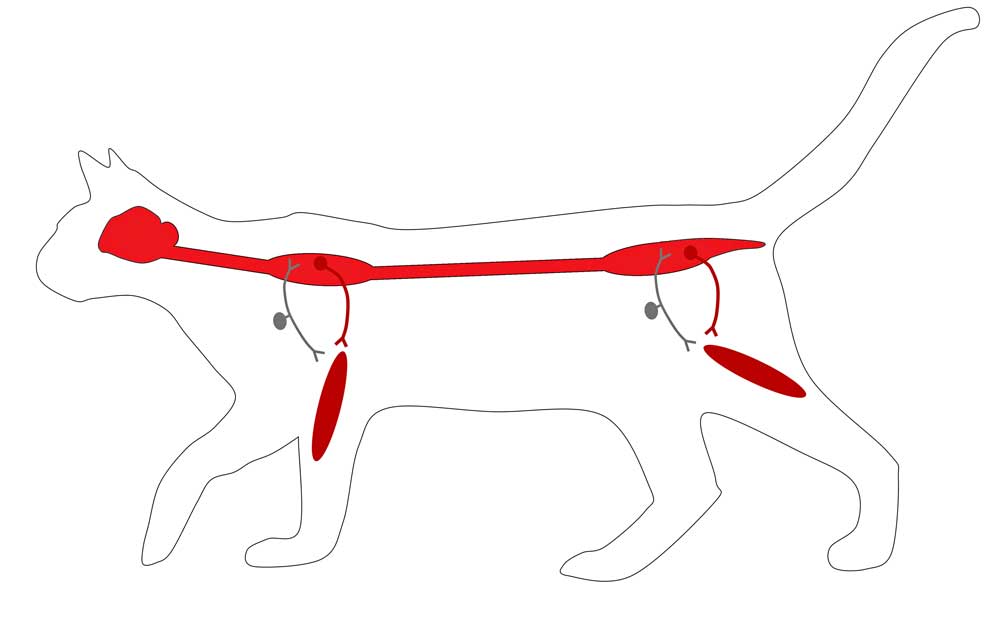
This results from a problem in the descending motor pathways; starting in the cerebrum, travelling down through the brainstem, spinal cord, motor nerve, neuromuscular junction and muscle (Figure 1).
Weakness can, therefore, result from any number of diseases – including neurological, orthopaedic and medical conditions.
Lameness is defined as a restriction to normal movement as the result of a focus of pain. Some use the term “mechanical lameness”, which is restricted movement of a joint due to a non-painful focus.
Lameness usually manifests as a shortened stride of the affected limb, with a longer stride in the contralateral limb.
Lameness is most commonly caused by orthopaedic disease, but neurological lameness is occasionally seen due to nerve entrapment – for example, from a tumour or a disc extrusion.
Neurological lameness is often accompanied by decreased tone in the limb, a reduced withdrawal reflex and marked atrophy.
Ataxia is best considered as incoordination – or to the uninitiated, “drunk”.
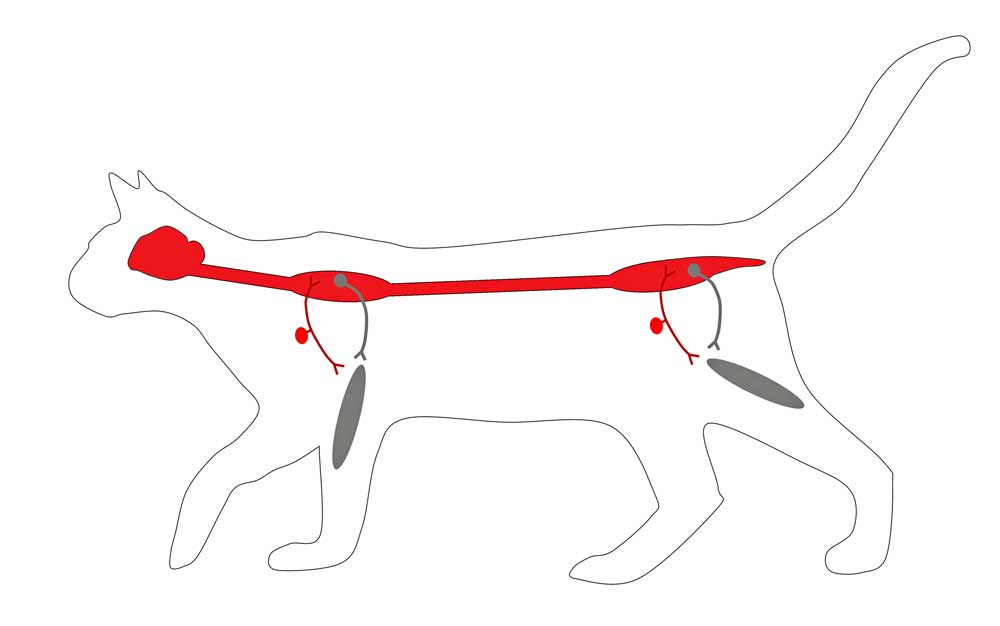
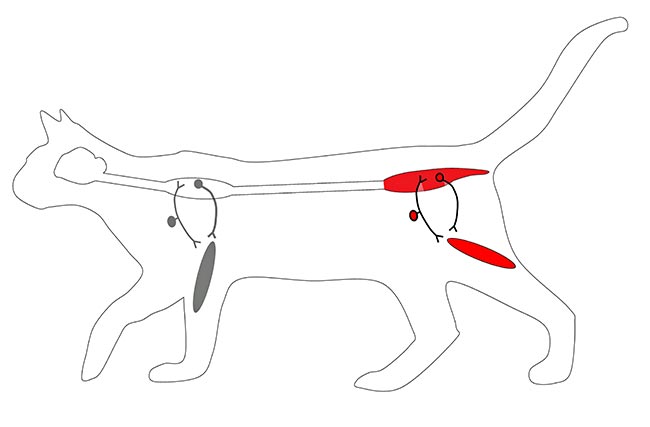
It is the result of a lesion in the ascending sensory pathway – starting from the sensory nerve, and ascending the spinal cord to the brainstem, cerebellum and cortex (Figure 2).
Ataxia has three distinct forms:
Cerebellar ataxia: the cerebellum acts to dampen movements and allow fine motor control. Absence of a cerebellum results in jerky exaggerated movements (hypermetria) reminiscent of the puppets from the 1960s classic TV series, Thunderbirds.
Vestibular ataxia: dysfunction of the vestibular system leads to cardinal signs of vestibular disease – for example, a head tilt, nystagmus and strabismus. Vestibular ataxia is differentiated from other forms of ataxia by its asymmetry. It is characterised by a broad‑based stance, swaying of the trunk and head, and falling to one side. If bilateral vestibular disease is present then falling/rolling to either side can occur with wide head excursions.
General proprioceptive/sensory ataxia: when ataxia is not defined by an asymmetry or exaggerated movements then it is most likely to be a general proprioceptive ataxia. This is commonly, but not exclusively, associated with disease of the spinal cord. Paresis is, therefore, often seen alongside the ataxia because the ascending and descending pathways are in close approximation – and so a lesion of one is likely to affect the other. In contrast, cerebellar and vestibular ataxias are less likely to be associated with paresis because the cerebellum and vestibular apparatus do not involve the motor (general somatic efferent) system.
The presence of ataxia is a very useful clinical sign because it implies a neurological problem and excludes orthopaedic conditions. This can be secondary to other conditions – for example, aortic thromboembolism resulting in an ischaemic neuromyopathy or hepatic insufficiency resulting in hepatic encephalopathy.
If the clinical examination and blood work can exclude such causes then a primary neurological condition is suspected.
Furthermore, the rarity of sensory nerve conditions means a brain or spinal cord condition should be considered and a neuromuscular problem can be excluded.
Having determined a neurological problem is present, it is important to determine how many limbs are affected. This, again, is aided by video footage of the cat in its own environment.
On occasion – particularly in cats that are non‑ambulatory – this question can be relatively straightforward to answer.
However, when managing ambulatory patients, it can be very difficult to distinguish subtle neurological signs in potentially affected limbs.
If a cat is obviously dragging a limb then postural reactions do not need to be assessed. However, if the results of gait observation are ambiguous, postural reactions are extremely useful to detect subclinical neurological signs.
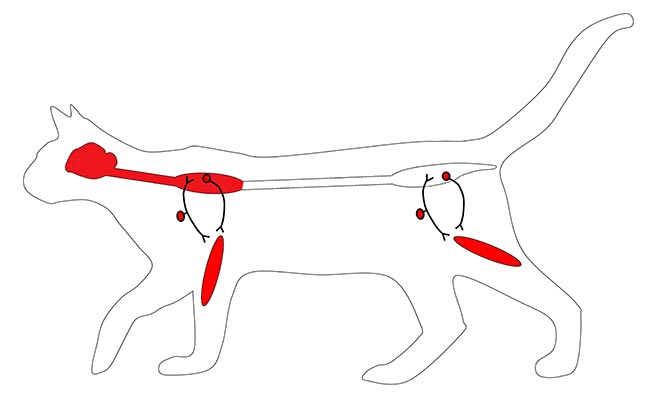
Postural reactions: the pathways involved in postural reactions incorporate the whole of the nervous system, and they reveal a cat’s awareness of its body and limb position, as well as the cat’s ability to generate movement. As such, they are non-specific for localising a lesion, but help to determine whether a particular limb is affected. Paw placement – or “knuckling” is commonly performed in dogs, but the author finds this unreliable and misleading in cats. Hopping and “wheelbarrowing” are more reliable, and the author’s first choice in all neurological cats (Figure 3). Tactile and visual placing can also be considered.

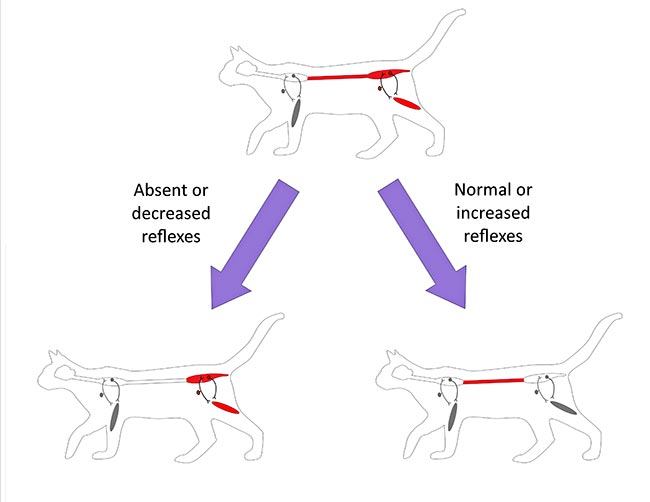
Performing the aforementioned tests should make it clear as to how many limbs are affected. Based on this information, the problem can start being localised:
If all four limbs are affected: the lesion is likely to be cranial to the T3 spinal cord segment or the lesion may relate to a generalised neuromuscular disease (for example, a polyneuropathy, polymyopathy or junctionopathy).
If the pelvic limbs are affected and the thoracic limbs are normal: this indicates a spinal cord lesion caudal to the T3 spinal cord segment, or a lesion of the pelvic limb, peripheral nerves or muscles (for example, neuromuscular disease).
If just one side of the body is affected: this is the same as for lesions affecting all four limbs, but the lesion is just on the affected side. A neuromuscular disease is unlikely in this circumstance, as these are usually bilaterally symmetrical.
If just one pelvic limb is affected: this is the same as for a lesion affecting both pelvic limbs, but the lesion is just on the affected side. A neuromuscular disease is unlikely in this circumstance, as these are usually bilaterally symmetrical.
If just one forelimb is affected: the lesion is likely to be on that side in the central grey matter of C6 to T2, the nerve roots, brachial plexus, peripheral nerves, neuromuscular junction or muscle.
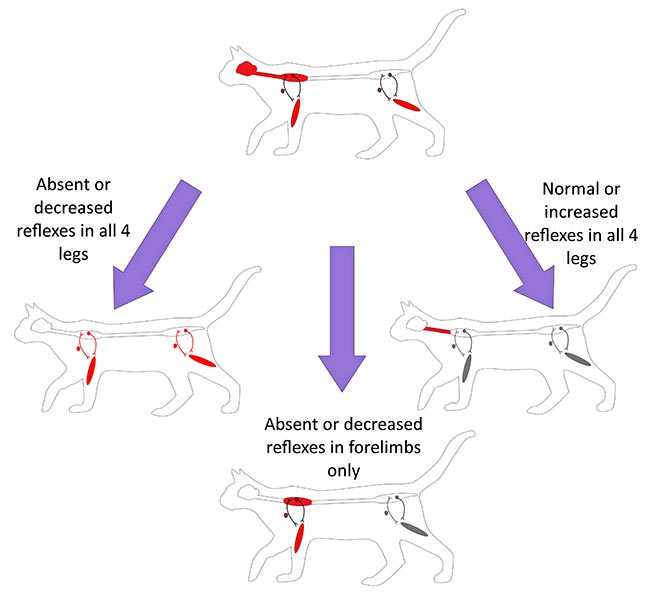
Now the limbs affected have been ascertained, a broad idea exists of where the lesion is likely to be. To narrow this localisation further, the cat’s reflexes in the affected limbs must be checked.
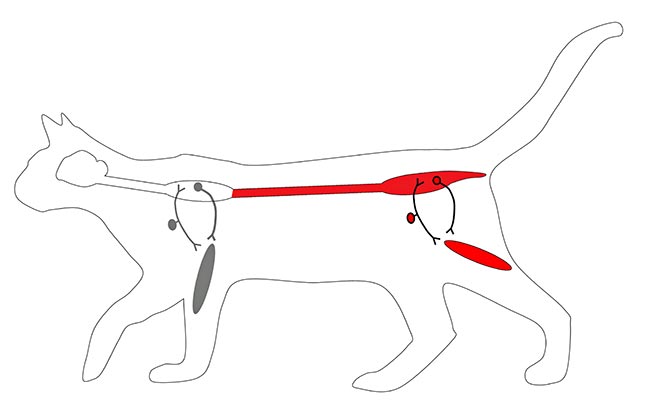
The author’s preferred reflex in cats is the withdrawal reflex (pedal or flexor reflex) as it evaluates multiple thoracic (C6 to T1) and pelvic (L6 to S1) limb nerves (Figure 4).

The patellar reflex can be considered and this evaluates the femoral nerve (L4 to L6). However, in the author’s opinion, the remainder of the spinal segmental reflex tests are unreliable; therefore, he does not perform them as part of a routine neurological assessment of the cat.
The suspected lesion locations based on reflexes are explained in Panel 1.
If all four legs are affected and the reflexes are normal or increased in all legs then a brain or C1 to C5 lesion is expected. If the reflexes are normal in the pelvic limbs, but decreased in the forelimbs, then a lesion affecting the C6 to T2 spinal segments is expected. Finally, if all four legs have decreased or absent reflexes then a neuromuscular localisation is expected:
Only a few select tests seem reasonable when performing a cranial nerve examination in cats. The two tests the author prioritises in a cat are the menace response and assessing for positional nystagmus.
The menace response is fairly non‑specific in aiding localisation of brain lesions, but is very good at detecting whether a brain lesion is present.
To test the menace response, a menacing gesture is made towards the tested eye (Figure 5). The normal response is a blink and potentially retraction of the head away from the stimulus. This is a learned response, so is only present from around 12 weeks of age in kittens.

The afferent part of this response involves the same structures as the visual pathways. The efferent part of the response is not well understood.
The information generated in the visual cortex is forwarded to the motor cortex to initiate a motor response. The corticobulbar pathways to the facial nerve nucleus, then transmits the motor information. This response requires intact facial nerve function as well as an intact cerebellum (ipsilateral function). The neuronal pathways through the cerebellum are not known.
Cats with a vestibular disorder can be perplexing and the vestibular ataxia can be difficult to detect.
Vestibular ataxia occurs with lesions affecting either the peripheral or central vestibular apparatus. Often the ataxia may manifest as a general proprioceptive ataxia limited to the pelvic limbs.
Cats with vestibular disease may have a broad-based gait (especially in the pelvic limbs) with leaning towards the side of decreased vestibular tone. Some cats may have substantial swaying when walking and will occasionally fall; recumbent cats may be seen to roll.
Weakness or paresis is only seen with central vestibular disease and is not a feature of peripheral vestibular disease.
In addition to ataxia, cats will often have concurrent neurological signs that reflect a vestibular disorder, such as head tilt (unilateral vestibular disorder) or head sway (bilateral vestibular disorder), pathological nystagmus or positional strabismus.
However, a number of cats will display nothing more than mild pelvic limb ataxia – and for this reason the author will test all ataxic cats for positional nystagmus (Figure 6). This is done by placing the cat upside down on its back, and extending its head and neck. The theory is it challenges the vestibular system – precipitating nystagmus, for which the cat is able to compensate to when positioned normally.

Having determined the localisation, it is possible to formulate a list of differential diagnosis using the “VITAMIN D” or “DAMNIT V” mnemonic for that particular neurolocalisation.
This will then allow you to determine the most appropriate diagnostic route to take, or, if the owner is unable to afford further investigations, give a clue as to the most likely diseases causing the clinical signs observed.