30 Apr 2024

Figure 1. Dogs with refractory epilepsy can often experience periods of time when they need to be admitted to hospital for anti-epileptic drug infusions. This can be a traumatic time for the owner and pet, and also adds to the financial burden of having an epileptic dog.
Epileptic seizures are one of the most common neurological signs in dogs, affecting approximately 0.6% to 0.75% of the general population (Berendt et al, 2015).
Epilepsy is a chronic condition, presenting acutely, that demands a high level of medical attention. Research has revealed a significant link between an owner’s perceived quality of life (QOL) for their dog and the frequency of monthly seizures, indicating an inverse relationship (Nettifee et al, 2017).
Furthermore, a decrease in a dog’s QOL is directly associated with a decrease in the owner’s QOL (Wessmann et al, 2016). Hence, it is crucial for all parties involved to optimise seizure management.
This article describes a step-wise approach to any epileptic canine patient failing to respond to anti-epileptic medication and offers guidance on different therapies available in such cases, with an emphasis on recent updates.
Pharmacoresistance, often referred to as drug-resistant epilepsy, regrettably represents a frequently encountered scenario, affecting up to 30% of dogs with epilepsy (Schwartz-Porsche et al, 1985).
It is characterised by the persistence of uncontrollable seizures, even when standard anti-epileptic drugs (AEDs) such as phenobarbital and potassium bromide are administered at appropriate doses, achieving appropriate therapeutic serum concentrations.
Refractory epilepsy (also known as pharmacoresistant epilepsy) defines dogs that have frequent and severe seizures despite appropriate drug therapy (that is, serum drug concentrations are at the high end of the therapeutic range), or have severe adverse effects from the anti-epileptic medication.
Refractory epilepsy can occur in as many as one in three epileptic dogs and is often challenging to manage (Schwartz-Porsche et al, 1985). This problem can increase the morbidity and mortality of this chronic condition, but it also places an increasing demand on the development of novel anti-epileptic treatments, as well as an added emotional and financial burden on the owner (Figure 1).

In some cases, it can be relatively straightforward to identify an epileptic seizure. However, on occasions, it can be much harder to determine whether the episode represents a seizure or something else.
Many non-epileptic paroxysmal disorders can mimic epilepsy, and in turn, this can mean the episodes are unresponsive to anti-epileptic drugs. Requesting videos of the episodes from owners is a helpful diagnostic tool. Other disorders that can resemble seizures include syncope, cataplexy (sudden muscle tone loss with intact consciousness), movement disorders (for example, myokymia, paroxysmal dyskinesia or tremors) and neuromuscular diseases leading to collapse.
Certain signs can help to distinguish a seizure from other forms of paroxysmal episode. Seizure-related signs often include autonomic signs (such as urination, defecation, and salivation), stereotypical characteristics, short seizure duration (usually less than a minute) and abnormal behaviour before or after the event (prodromal or post-ictal phase).
Dogs with seizures affecting all four limbs would also be expected to lose awareness during the episode rather than remain conscious. Complete unresponsiveness to anti-epileptic medication is uncommon, as refractory epileptic patients often initially show improvement, but may later develop tolerance or experience adverse effects.
Once the abnormal episodes have been established as epileptic seizures, the next step is to try to identify the underlying cause.
A dog failing to respond to therapy may have an identifiable underlying cause for the seizures. The dog might have recently developed seizures and the medication is failing due to a progressive underlying disease process (for example, intra-cranial tumour or inflammatory brain disease).
Alternatively, the patient may have a long-term history of seizures that were once managed successfully with medication, but now “break-through” seizures are occurring.
To avoid these problems, it is worth reviewing the history and diagnosis of each individual case. Seizures are broadly grouped into “intra-cranial” and “extra-cranial” causes (Panels 1 and 2).
Metabolic
Toxic
Vascular
Inflammatory
Anomalous
Degenerative
It is recommended to initiate the diagnostic process with routine blood tests to investigate potential metabolic (extra-cranial) causes.
Optimal results are obtained when the dog has fasted for 12 hours prior to blood sampling. In situations where this is not feasible, scheduling blood sampling for the following day might be a viable alternative.
Some of the following tests are particularly important and should be considered:
A neurological examination should be repeated in a patient with refractory epilepsy to ensure no change has occurred since first assessment.
If an intra-cranial cause for the seizures is present, it is possible that subtle neurological deficits not visible at first evaluation have now progressed and become more obvious.
Neurological deficits should be consistent with forebrain dysfunction and may include mentation changes, central blindness (a decreased to absent menace response with an intact pupillary light reflex), frantic pacing and general proprioceptive ataxia (appearing to have a drunken gait).
Note that all these signs can be seen in the post-ictal period (usually for up to 24 to 48 hours), although they would then tend to be symmetrical in nature. Therefore, repeating the neurological examination at least 48 hours after a seizure is recommended whenever possible.
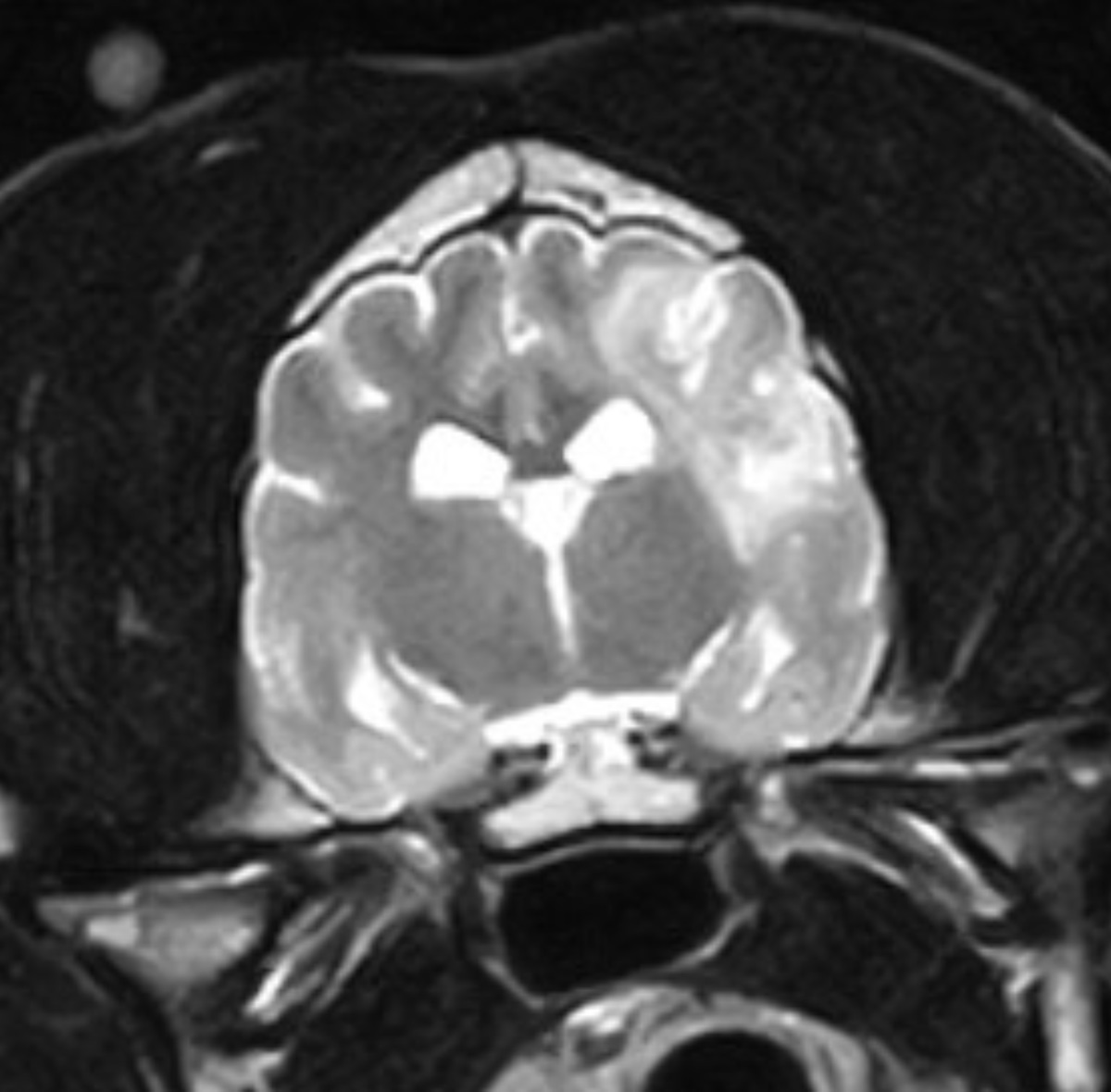
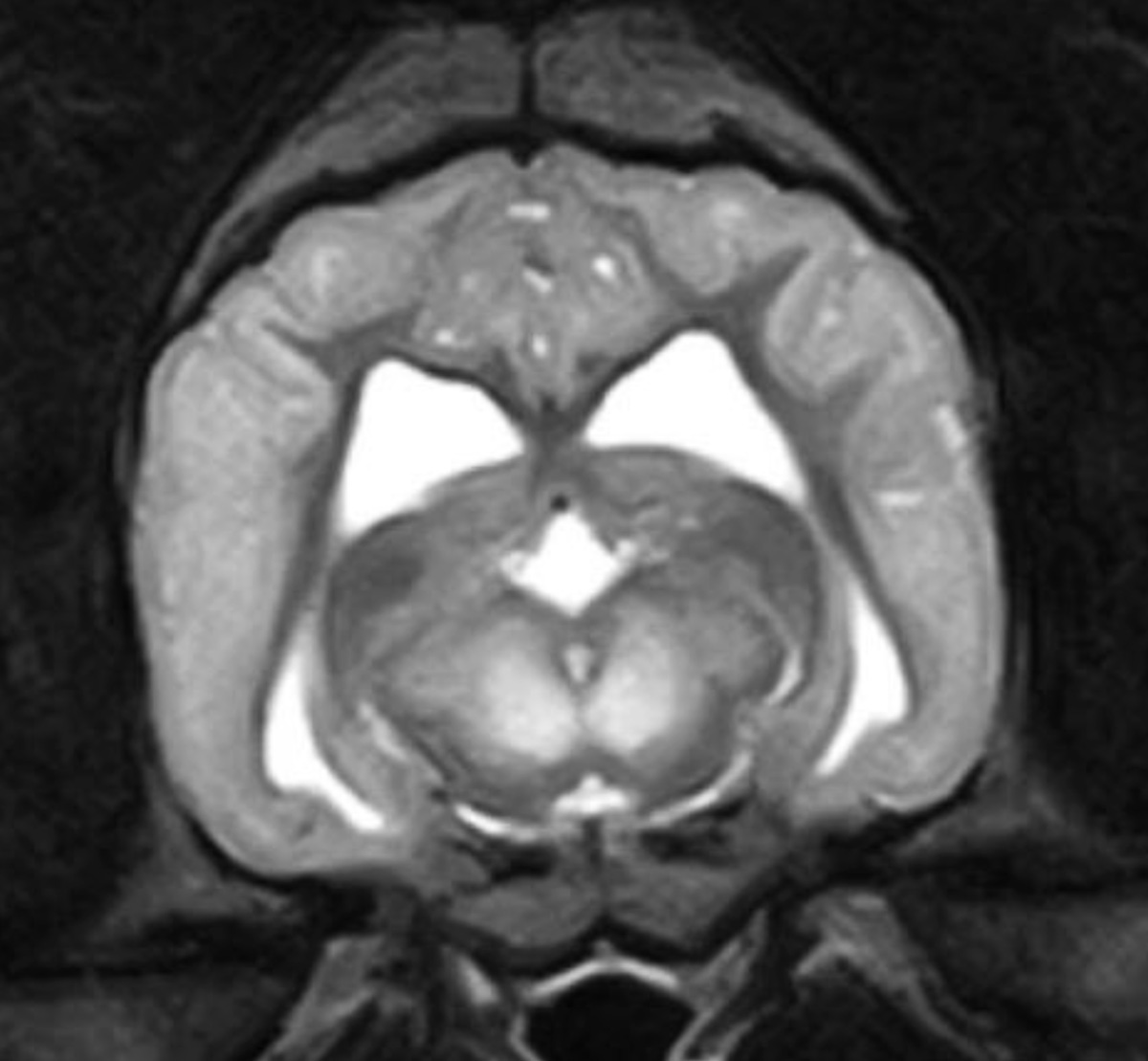
If any abnormalities are detected then advanced imaging of the brain is advised. Additionally, a normal neurological examination does not infer a normal brain, and so advanced imaging should always be considered in a refractory epileptic patient. Similarly, advanced imaging is recommended in any dog with an abnormal neurological examination (Figures 2 and 3).
Inappropriate dosing of anti-epileptic medication is a common reason for break-through seizures to occur. Serum concentrations must be monitored regularly (every six months) to ensure they are within the therapeutic range.
However, if the patient is in the sub-therapeutic range and the seizures are well controlled, then no need exists to increase the dose of medication.
The following medications can be considered in canine epilepsy.
Monotherapy with phenobarbital, at an initial dose of 2mg/kg to 3mg/kg every 12 hours, gives effective control for the majority of epileptic dogs providing that therapeutic serum concentrations are maintained. It is estimated that 60% to 80% of dogs on phenobarbital monotherapy are effectively controlled. Auto-induction occurs with long-term phenobarbital use (that is, increased metabolism of the drug with time).
To maintain the therapeutic serum concentration, subsequent increases in dose may be required. This is due to hepatic enzyme induction that decreases the elimination half-life of the drug.
Auto-induction, therefore, means that many patients may eventually require a dose that is much higher than the starting dose. The half-life of this drug is, therefore, very variable, being between 40 to 90 hours, meaning it takes 10 to 14 days to reach steady state. Timing of blood sampling for phenobarbital serum concentrations should be two weeks after any dose change. However, consistency as to when this sample is collected in relation to timing post-pill is an important factor.
Potassium bromide may be used as sole therapy or in conjunction with other AEDs. It is particularly beneficial in dogs with sub-optimal control on phenobarbital alone, as these two AEDs together provide a synergistic effect.
It is also useful for dogs with hepatic insufficiency due to its exclusively renal excretion.
A major disadvantage of potassium bromide is that it takes three to four months to achieve steady-state concentrations when started at maintenance doses; therefore, serum concentration should only be measured after this time has elapsed. Longer-term routine blood monitoring is recommended every 6 to 12 months.
If used to control frequent or severe seizures, a loading protocol may be required to reach steady-state concentrations more quickly; for example, a common protocol is to administer 600mg/kg orally divided over 5 days and measure serum concentration 24 hours later.
Hospitalisation while loading is preferable due to the possibility of developing severe side effects, including sedation, ataxia and vomiting.
Imepitoin is a relatively recent addition to the array of AEDs available for canine epilepsy. It is specifically indicated for monotherapy in dogs with idiopathic epilepsy experiencing recurrent single generalised seizures.
A study involving 226 dogs revealed that imepitoin, administered twice daily at incremental doses of 10mg/kg, 20mg/kg or 30mg/kg, demonstrated comparable efficacy to phenobarbital (Tipold et al, 2015). Moreover, the imepitoin group experienced significantly fewer side effects than the phenobarbital group. In contrast, a more recent study (Stabile et al, 2019) looked at dogs given either imepitoin (n=31) or phenobarbital (n=30) as monotherapy for epilepsy. The study involved 31 dogs receiving imepitoin and 30 receiving phenobarbital, with dosages adjusted over time.
It was found that 67.7% dogs receiving imepitoin developed cluster seizures versus 36.7% in the phenobarbital group. In the imepitoin group, 9.7% did not develop cluster seizures over the three-year follow-up versus 63.3% in the phenobarbital group. A total of 23% of dogs on imepitoin experienced adverse events, necessitating a switch to another medication.
These results suggest that dogs with idiopathic epilepsy given first-line treatment with imepitoin may experience cluster seizures more frequently and earlier, along with adverse effects such as aggression and the need for earlier discontinuation, compared to those on phenobarbital monotherapy. Regular monitoring through haematology and biochemistry is recommended every 6 to 12 months for dogs on imepitoin.
However, the overall monitoring process for patients on imepitoin is likely to be less expensive compared to those on phenobarbital. It is important to note that insufficient evidence exists to support the use of imepitoin as an add-on AED or in cases of cluster seizures or status epilepticus.
Levetiracetam is a well-tolerated medication that is particularly useful as an add-on AED in cases of refractory epilepsy, although it is not licensed for use in dogs. Similar to potassium bromide, its primary route of excretion is via the kidneys, making it a suitable choice for dogs with liver dysfunction. In circumstances where dogs have cluster seizures followed by long intervals of seizure freedom, it might be worth considering “pulse therapy”.
An initial dose of 60mg/kg is followed by 20mg/kg every 8 hours for the duration of the cluster and may be stopped altogether once the dog has been without a seizure for 48 hours.
“The aim of therapy is to restore a normal life for the pet and family, with no adverse drug effects.”
It is useful for owners to have rectal diazepam available at home – particularly for dogs that are prone to having cluster seizures. The recommended dose is 0.5mg/kg to 2mg/kg and may be repeated to a maximum of 3 administrations within 24 hours.
For the majority of epileptic dogs, the AEDs described previously, either alone or in combination, will be sufficient to provide effective seizure control. For refractory cases in which the seizures remain frequent or severe, other options are available, such as gabapentin, felbamate, topiramate and zonisamide.
Some of these AEDs are associated with a relative lack of clinical evidence to support their efficacy. Some may also be prohibitively expensive – particularly for large breeds of dog.
It is important to note that if a dog’s epilepsy is so severe as to need to consider one of these medications, it is unlikely the new medication will be the “magic bullet” that leads to a significant improvement.
At this stage, it is important to establish the client’s expectations. The aim of therapy is to restore a normal life for the pet and family, with no adverse drug effects. However, in reality, achieving this goal is often extremely difficult.
A better approach is to aim at reducing seizure severity and frequency to a level that does not substantially compromise the QOL for the dog and family, while trying to avoid adverse drug effects. These points are crucial to success, as further medications can be expensive and require a solid commitment from the owner, with the understanding that acceptable control for a patient may constitute a reduction in seizure frequency of 50% (which may equate to 5 seizures per month instead of 10).
Client compliance is a factor that must be considered in the management of refractory epileptics. It is important to ensure the drugs are given appropriately, at the correct time and dosage, and that the clients have not adjusted the dose based on a short-term assessment of seizure control or side effects.
If you are presented with a dog with idiopathic epilepsy, it is important the client understands what the problem is and why it has been difficult to manage their dog’s seizures. Historically, the focus with idiopathic epilepsy has been on diagnosing and treating the condition, but increasingly, a recognition exists of the profound impact canine epilepsy has on the lives of dog owners.
The following key areas should be considered.
Effective communication from the initial consultation is vital. Guiding owners toward resources to understand and navigate the care required for an epileptic dog positively influences owner QOL.
Owners should be well-informed and empowered to be active caretakers of their pets. Informed decisions and effective veterinarian-client communication can make a world of difference.
We need to consider the impact of caring for a chronically ill pet on the lives of our clients. Managing long-term conditions can be emotionally challenging, reminiscent of the experiences of caregivers in human medicine.
Owners of dogs with idiopathic epilepsy often shoulder a significant burden. Watching their pets endure seizures, coping with medication side effects, and navigating the post-ictal period can be emotionally distressing. Moreover, the degree of success in controlling seizures does not always correspond with the owner’s dedication, leading to a sense of helplessness.
The emotional and financial burdens, time constraints, lack of sleep, and social isolation all take a toll on their QOL. The emotional impact is especially significant, often exceeding expectations, and it is even more pronounced when the dog’s seizures are poorly controlled.
Given that many dogs can be refractory, and anti-epileptic medication may be limited in its efficacy, it seems unsurprising that owners will explore alternative options.
These alternative management strategies have a varying evidence base. Some of these treatments are listed with the relevant information given.
Cannabis comprises numerous cannabinoids, with cannabidiol (CBD) being the primary non-psychoactive compound, and tetrahydrocannabinol (THC) being the primary psychoactive compound. Anti-epileptic properties are attributed to CBD, prompting suppliers of medicinal cannabis to target increased levels of CBD and minimal THC in the compounds they supply.
The subject of CBD is frequently raised by owners of epileptic dogs. To date, only two clinical trials have been conducted assessing the use of CBD in dogs with refractory epilepsy in addition to conventional AEDs.
In the first, a significant decrease in seizure frequency (33%) was seen in dogs given CBD oil compared to those in the placebo group (McGrath et al, 2019). However, this was slightly tempered by the fact that 50% of dogs in both groups were considered responders, experiencing a 50% reduction in seizure activity. The CBD group exhibited a significant increase in serum alkaline phosphatase levels, and side effects included ataxia.
In the second study, the number of responders with a reduction in seizure frequency less than or equal to 50% amounted to 6 of 14 dogs in the CBD group, whereas a respective reduction was not observed while these same dogs were on placebo (Morrow and Belshaw, 2020).

Image © Nynke / Adobe Stock
The ketogenic diet, first acknowledged for its efficacy in managing epilepsy in humans in 1921, spurred the development of the medium-chain triglyceride (MCT) diet as a more palatable alternative.
The MCT diet substitutes medium-chain fatty acids for a portion of the long-chain fatty acids in the classic ketogenic diet. This modification is based on the premise that MCTs are efficiently absorbed from the gastrointestinal tract and are more ketogenic than long-chain triglycerides, thereby allowing more carbohydrate in the diet without compromising the ketogenic basis. Noteworthy results emerged in dogs with chronic idiopathic epilepsy, where those fed a 5.5% MCT diet experienced significantly lower seizure frequency compared to those without the diet (Law et al, 2015).
An interesting commercial counterpart is the Purina Pro Plan Canine NC Neurocare diet, which contains 6.5% MCT, resembling the formulations used in research. This diet was evaluated in dogs with idiopathic epilepsy, which did not suffer cluster seizures.
The diet yielded a 32% reduction in monthly seizure frequency compared to the month immediately preceding the start of the supplement, highlighting the potential of MCT-based diets and MCT oil as a promising avenue in managing epilepsy in dogs (Molina et al, 2020).
Two methods of vagal stimulation have been trialled in dogs to produce an anti-epileptic effect, one of which involves the placement of a pacemaker-like device delivering intermittent stimulation to the vagus nerve. This method currently has limited clinical use due to its restricted availability, expense and invasiveness.
The other is a more crude technique involving digital ocular compression, which has been shown to abort or prevent seizures in some dogs.
The placebo effect is a well-recognised, but poorly understood, phenomenon that involves a non-specific psychological or physiological therapeutic effect of a medical intervention that lacks specific activity for the condition being treated.
A decrease in seizure frequency was seen in more than half of the dogs administered a placebo when compared with baseline values (Muñana et al, 2010). Almost 30% of these dogs could be classified as responders when based on a 50% or greater reduction in seizure frequency.
The conclusion drawn from this study is that the efficacy of any anti-epileptic therapy can only be evaluated accurately when using placebo-controlled trials.
This article serves as a practical handbook for handling drug-resistant epilepsy in dogs.
It provides guidance on extracting crucial information from the signalment, history and a targeted examination to ascertain whether the observed episodes align with epileptic seizures, and to pinpoint potential differential diagnoses. By doing so, it aids in prioritising diagnostic tests and determining the appropriate course of management.
The article underscores the significance of managing client expectations and acknowledging the emotional and financial challenges faced by owners.
By addressing expectations early on, it enables the implementation of effective management, recognising that unrealistic expectations often lead to perceived treatment failure.
Furthermore, the exploration of alternative therapies underscores the ongoing quest for more effective approaches.